As the endoscope is guided down, the narrow esophageal passage opens up into the stomach. The delicate pink tissue glistens with mucus but in places red pinpricks and patches of inflamed tissue are clearly visible. The doctor’s diagnosis? Gastritis.
Though it looks so painful, some people with the condition will have few symptoms. Unfortunately, others will experience pain or discomfort in the upper abdomen, explains Dr. Anuja Somaratne, Consultant Surgeon. If neglected, severe cases can develop chronic stomach ulcers which can eventually lead to stomach cancer. This week Dr. Somaratne speaks to MediScene about what causes the condition and how it can be cured.
An inflammation in
the mucosa
The stomach boasts a thick lining known as the mucosa, explains Dr. Somaratne. Containing special cells that produce acid and enzymes, which help break down food for digestion, the mucosa also has mucus, which protects the stomach lining from acid produced by the stomach. In someone with gastritis, this lining is inflamed.
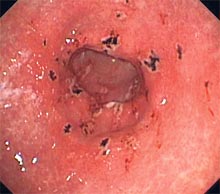
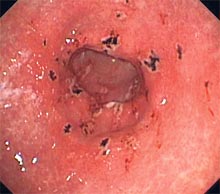 |
| Gastritis with erosions |
Sudden, severe inflammation of the stomach lining is called acute gastritis; in contrast, chronic gastritis is diagnosed when the inflammation is of a longer duration. If left untreated, chronic gastritis can last for years.
A few patients may also suffer from what is known as erosive gastritis. This type of gastritis often does not cause significant inflammation but it still wears away at the stomach lining causing erosions, bleeding or ulcers. Erosive gastritis may be acute or chronic.
If you’ve experienced pain or discomfort in your abdomen, you may have been tempted to label it gastritis. But it is worth noting that many other diseases and disorders may be associated with these symptoms. It’s best to consult with a doctor to see what ails you.
From bacteria to burns
A tiny bacterium is one of the best known causes of gastritis. Infecting your stomach or the first part of your small intestine, H. pylori is exceedingly common. Many will harbour the bacterium without feeling any side effects, but for some H. pylori infections result in ulcers and stomach cancer. It is particularly common in those living in areas with poor sanitation because it can be transmitted through contaminated food or water.
Another common cause are what are known as nonsteroidal anti-inflammatory drugs (NSAIDs). Painkillers such as aspirin and ibuprofen are known to trigger erosive gastritis – both acute and chronic. Other agents that can cause erosive gastritis include alcohol, cocaine and chronic bile reflux, says Dr. Somaratne, going on to identify alcohol abuse as one of the most common causes.
Physical trauma can also lie at the heart of a gastritis attack. Known as stress gastritis, it is caused by injuries, critical illness, severe burns, and major surgery. Among the lesser known causes of gastritis are autoimmune disorders (in which the immune system attacks healthy cells in the stomach lining) and digestive diseases and disorders, such as Crohn’s disease and pernicious anemia.
Symptoms and
complications:
In those who do experience symptoms, gastritis can manifest as upper abdominal discomfort or pain, accompanied by nausea and vomiting, says Dr. Somaratne. These symptoms are dyspepsia. Blood in your vomit or blood in your stools (it can also manifest as black, tarry stools) is a sign that ulcers or erosions in your stomach caused by erosive gastritis have penetrated the stomach lining. The resulting bleeding is a sign that it’s time to visit a doctor.
If left untended for a long period, chronic gastritis is considered a risk factor for peptic ulcer disease, gastric polyps, and gastric tumours.
Diagnosing Gastritis:
An endoscopy is the most common diagnostic test for gastritis and may include a biopsy of the stomach lining. The long, thin tube with a camera at one end is inserted through the mouth. The endoscope allows a doctor to see the state of your stomach for himself. In anxious patients, sedation can be used - general anaesthesia rarely so, as a local anaesthetic spray into throat suffices for most. If necessary, the doctor will use the endoscope to perform a biopsy, which involves collecting tiny samples of tissue for examination with a microscope. Endoscopy requires a four to five hours of fasting done as out-patient basis.
Other tests used to identify the cause of gastritis or any complications include Upper gastrointestinal (GI) series which utilize X-Rays, blood tests and stool tests. Your doctor might also choose to test for H. pylori infection.
Treating Gastritis:
Medications that reduce the amount of acid in the stomach can relieve symptoms that may accompany gastritis and promote healing of the stomach lining. These include antacids (which relieve mild heartburn or dyspepsia by neutralizing acid in the stomach) and histamine 2 (H2) blockers that decrease acid production. Proton pump inhibitors (PPIs) are also used to decrease acid production and prevent stress gastritis in critically ill patients.
If gastritis is caused by prolonged use of NSAIDs, a doctor may recommend another class of medications for pain. Treating H. pylori infections is important, even if a person is not experiencing symptoms from the infection. Some untreated H. pylori gastritis may lead to cancer or the development of ulcers in the stomach.
After treatment, the doctor may use a breath or stool test to make sure the H. pylori infection is gone. Curing the infection can be expected to cure the gastritis and decrease the risk of other gastrointestinal diseases associated with gastritis, such as peptic ulcer disease, gastric cancer.
Gastritis at a glance
Gastritis is a condition in which the stomach lining is inflamed.
The most common causes of gastritis are H. pylori infections and prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs).
Many people with gastritis have no symptoms. Those who do have symptoms may experience dyspepsia—upper abdominal discomfort or pain, nausea, or vomiting.
Treating H. pylori infection is important, even if a person is not experiencing symptoms. Left untreated, H. pylori infection may lead to peptic ulcer disease or cancer.
Foods to avoid
Alcohol, black and red pepper, chillies, chilli powder, and hot peppers often irritate the stomach lining. Foods with caffeine can increase the amount of stomach acid.
These foods include coffee (regular and decaf), teas, colas, cocoa, chocolate. Avoid or limit these items if they cause you pain.
Limit your intake of tomatoes, tomato juice, peppermint, fatty foods, and citrus juices. If they cause heartburn or pain in your esophagus. You may need to limit seasonings such as onions, garlic, cinnamon, and cloves if they upset your stomach.
Dietary fibre
Eating high fibre foods does not worsen stomach pain for most people with ulcers or gastritis. High fibre foods include whole grains, cooked dried beans, and fruits and vegetables with peels.
You may notice that some foods can cause you to have extra gas. This may include, cabbage, onions, milk and some fruits. Pay attention to the foods that cause you trouble, and limit or avoid them according to how you feel. |