How low do you feel?
I’ll change my state with any wretch,
Thou canst from gaol or dunghill fetch;
My pain’s past cure, another hell,
I may not in this torment dwell!
Now desperate I hate my life,
Lend me a halter or a knife;
All my griefs to this are jolly,
Naught so damn’d as melancholy.
Robert Burton – Anatomy of Melancholy
Robert Burton was a Dean of Divinity at Oxford and his Anatomy of Melancholy published in 1621 is a superb literary description of a pathological mental state. Burton himself suffered a classic case of melancholia. Most of what he knew about mental illness was derived from his own inner experiences. He ended his life by hanging himself in his rooms in Oxford.
Melancholy or melancholia comes from the old medical belief that disease was caused by an imbalance of the four humours (blood, phlegm, black and yellow bile) in the body. According to Hippocrates, melancholia was due to an excess of black bile hence the name which means black bile in ancient Greek, ‘melas’ black and ‘khole’, bile. In modern terminology melancholia is the term used to describe a severe depression.

Depression has many faces. Pic by M.A. Pushpa Kumara
Passing moments of feeling sad, down or depressed are a part of the human condition. These episodes are usually in relation to day-to-day problems of life and resolve spontaneously in a short period of time. What do we know of depression today? The term is a misnomer. By depression we do not mean such transient episodes of sadness. The medical use of the term denotes a syndrome or collection of symptoms that constitute what doctors call a depressive disorder. I will use the term depression in this sense.
Clinical depression is persistent, impairs day-to-day functioning and includes a range of symptoms. There are different types of depression of which the most important is called, in psychiatric jargon, major depressive disorder (MDD). In MDD the main symptoms are a sad or low mood, loss of interest and pleasure in almost everything the person used to enjoy in the past. These include food, sex, work and being with family and friends. The symptoms are persistent and are present almost daily and should last for two weeks or more. There may also be accompanying physical symptoms such as disturbance in appetite (loss or increase in appetite), changes in weight (loss or increase in weight), sleep disturbance (trouble falling asleep, waking up in the middle of the night and not being able to go back to sleep, waking up early in the morning and feeling dreadful).
There may be other symptoms such as a feeling of restlessness (being unable to sit still, pacing or hand wringing) or lethargy (slowness of speech and movements). Reduced energy, a feeling of tiredness and fatigue are also common. The tiredness is independent of physical exertion. Even little tasks require a great deal of effort and more time than before. Many persons with depression also report difficulty with concentration. They are easily distracted and complain of memory problems. In students this may lead to a fall in academic performance and in the elderly the memory loss may be sufficiently severe to be mistaken for early signs of dementia. This is termed pseudodementia.
Thoughts of death, feeling that life is not worth living, ideas of suicide or even suicide attempts are features of depression. These thoughts of dying may range from a passive wish to not awaken in the morning or die of an accident or illness to contemplation of ways of committing suicide. Severely depressed persons may proceed to active planning to end their life by collecting tablets or poisons and put their affairs in order by writing wills, paying off debts or giving away their possessions. Such behaviours may be a warning sign to family members and friends of impending suicide. I remember the story told me by another psychiatrist where a medical student suddenly decided to give away his valuable wristwatch to his best friend. Fortunately his friend who also happened to be a medical student was alert enough to question him further to find that his friend was severely depressed and was contemplating suicide. He was treated and his life was saved.
It is not necessary to have all the symptoms described above to have a clinical depression. If you have five or more symptoms persisting for several weeks that result in impaired ability to take care of yourself or your family, or cause significant problems in your working life, then you probably have a major depressive disorder.
MDD is the main type of depression but it is not the only type. In children depression can present quite differently with severe recurrent outbursts of temper with physical and verbal aggression to people and property, grossly out of proportion to the situation or provocation. These outbursts on average occur around three or more times per week and in between these outbursts the mood is irritable or angry most of the time. It is important to diagnose and treat this condition as otherwise it would lead to serious disruption of schoolwork with the risk of progressing to adult type of depression in later years.
Another more severe form of depression is called psychotic depression. In this form there is, in addition to the features described for MDD, distortion of thinking. Persons with such depression feel guilty and blame themselves for perceived wrongs. They may also feel that the depression was brought about because they have been bad or done a crime. Though not common it is important to identify this kind of depression as it needs urgent medication and will not respond to psychotherapy.
A more common form of depression is mild depression or dysthymia. Such patients have milder symptoms than those with MDD, for example difficulties in sleeping and loss of interest.
These are persistent and for a definitive diagnosis should have lasted for more than two years in the case of adults, and one year in children and adolescents. Though symptoms are less severe than for MDD it is still important to diagnose this condition as it can seriously impair enjoyment of life and productivity. Also these individuals are more likely to develop MDD in later life.
In some, depression is a part of another psychiatric disorder called bipolar disorder. In individuals with bipolar disorder in addition to episodes of depression they also suffer from manic episodes. In manic episodes the mood is elevated, expansive or irritable. There is increased activity, racing thoughts, feeling of excessive power (grandiosity), unrealistically high self-esteem and easy distractibility. Such individuals also get involved in activities with potential for damaging consequences such as excessive spending, abuse of drugs and alcohol and sexual excesses. It is important to identify bipolar disorder as it is usually a lifetime affliction with serious negative consequences health-wise and socially. The treatment is different and more complicated than for depression.
The causes of depression
In the past depression was divided into two types, endogenous or biological depression and reactive depression. Endogenous depression is mainly due to biological or genetic factors and reactive depression to adverse life circumstances. However it is now recognised that depression in most cases is due to a combination of biological factors and problems in the environment.
Is depression inherited? First degree family members of individuals with depression have two to four fold higher risk of developing the condition than the general population. There is no single gene that determines whether you get depressed or not but it is the inheritance of ‘neurotic’ personality traits that increase the vulnerability to depression.
How to know whether you are depressed?
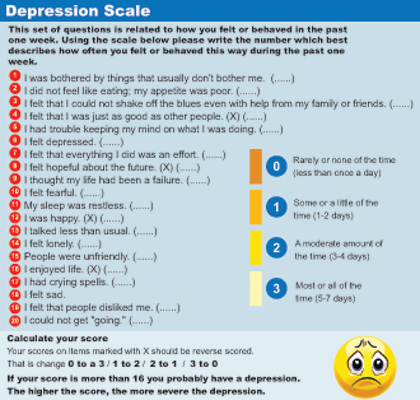
If you feel you have the features given here of a depression it is best to see a psychiatrist to confirm or to start on treatment. But here is a standard questionnaire that you can use to determine your overall depression score. This questionnaire is called the Centre for Epidemiologic Studies Depression Scale or CES-D for short.