News
Live telecast of robotic surgery a first at joint sessions of UK-Lanka urologists
Robotic surgery in Sri Lanka, not in an operating theatre of a local hospital, but streamed-in live from England to a distinguished gathering. This surgery known as ‘going beyond human hands’, is being telecast live from Essex, the time there being 10 a.m. and in Sri Lanka 3.30 p.m. on Monday (November 4).
“It’s like playing video games, we joke, because there has to be good eye-hand coordination,” says Consultant Urological Surgeon, Dr. Ranjan Thilagarajah, while manning the consoles of the robotic surgery instrument at the Broomfield Hospital.
Step-by-step he goes through the robotic surgical procedure to remove a large stone (about 3cm) from the left kidney of a woman patient, as both locals and foreigners remain glued to the screen on the 12th Floor of the Asiri Surgical Hospital at Narahenpita.
The live telecast of the robotic procedure is a unique part of the joint sessions, also a first, between the Sri Lanka Association of Urological Surgeons (SLAUS) and the British Association of Urological Surgeons (BAUS) this week. On Wednesday (November 6), at the inauguration of the 8th Annual Academic Sessions of SLAUS at the Taj Samudra Hotel, SLAUS President Dr. Anura Wijewardane says the joint sessions are “a landmark meeting” in reviving and rejuvenating the closeness between the United Kingdom and Sri Lanka in the field of urology.

From left SLAUS Secretary Dr. Ajith Malalasekera, Guest-of-Honour Dr. Athula Kahandaliyane, Chief Guest and BAUS President Mark Speakman and SLAUS President Dr. Anura Wijewardane. Pix by Nilan Maligaspe
The chief guest at the inauguration was BAUS President Mark J. Speakman and the guest-of-honour, the World Health Organization’s Southeast Asia Region’s Sustainable Development and Healthy Environment Director Dr. Athula Kahandaliyanage.
Tracing the development of urological treatment in the country, Dr. Wijewardane laments that although laparoscopic urology was introduced about a decade ago, it is not widely available and practised in Sri Lanka. He is confident, however, that with the expansion of the consultant cadre and the arrival of the younger generation of urologists, laparoscopic urology would be established in the near future.Referring to the “many challenges” faced by Sri Lanka’s urologists with regard to technology and manpower, he says that there are urology centres with a shortage of theatre time, trained supporting staff and equipment. “At times, the state sector is very frustrating to the well-trained, young urologist as they have to transfer their patients elsewhere due to lack of facilities.”
Citing the example of only three extracorporeal shock wave lithotripsy (ESWL) machines being available in only two of the nine provinces, he reiterates that it is insufficient to provide treatment to the increasing number of patients. (ESWL is non-invasive treatment for stones in the kidney or gall bladder.)
“We have now proposed to raise funds to purchase a mobile lithotripter to provide services to the other seven provinces,” he said, adding, “This is a challenging task as the cost in rupees is enormous.” Detailing the work done by SLAUS, Dr. Wijewardane points out that under the theme, ‘Spreading the knowledge of urology’ initiatives have been taken to create awareness on the management of common urological conditions.
For a population of just over 20 million, there are 23 practising urologists. Outside Colombo, there is a notable shortage of urologists. In seven of the nine provinces, there are more than one million people per urologist,” he points out, adding that all urological services outside Colombo are provided only by State-sector urologists and the number is insufficient.
“Hence it is our responsibility to provide adequate training opportunities and we are very keen to facilitate an overseas training scheme through BAUS. Our association wishes to explore the opportunities in Britain for our trainees in the areas of neuro-urology, reconstructive urology, laparoscopic urology and andrology,” he said.
Dr. Wijewardane also invited suggestions from BAUS on how Sri Lankan urologists could contribute to the training of those in the UK, probably in the areas of stone surgery and open urological surgery, due to the high turnover in Sri Lanka.
Demonstrating how the urologists’ role extends far beyond the kidney, ureter, bladder and male genitalia, Dr. Wijewardane said that common urological diseases are closely associated with all the components of metabolic syndrome. It has been found to be associated with a number of urological diseases including urolithiasis (urinary stones), benign prostatic hyperplasia, erectile dysfunction, male infertility, female incontinence and cancer of the prostate.
As such all urologists need to be cognizant of the impact that metabolic syndrome has on urological disease as well as on the patient’s overall health, says Dr. Wijewardane citing the Chinese proverb, “A superior doctor prevents illness, a mediocre doctor attends to impending illness and an inferior doctor treats actual illness”.
Traditional as against computer assisted surgery
Magnification is one of the best advantages of robotic surgery, said Urological Surgeon Dr. Ranjan Thilagarajah, explaining that this minimally-invasive or key-hole surgery allows micro-dissections while providing a three-dimensional vision.
It is performed through a few small incisions instead of a large cut across the abdomen, the Sunday Times learns, reducing the pain and time in hospital for the patient.
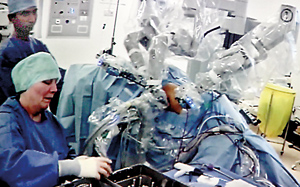
Contrasting robotic surgery with traditional laparoscopy, Dr. Thilagarajah (who is of Sri Lankan origin) says that the robotic instrument allows normal wrist movements whereas in laparoscopy the instruments are straight. The wrist movements come in handy especially in stitching.
In traditional laparoscopic surgery, long-handled surgical instruments including a tiny camera are inserted through the cuts and the camera transmits images to a video monitor for surgeons to view during the procedure, it is learnt.
Robotic surgery, meanwhile, includes a magnified 3D high-definition vision system and special wristed instruments that bend and rotate far greater than the human wrist. This enables the surgeon to operate with enhanced vision, precision, dexterity and control, research reveals.
At Monday’s “live” robotic surgery session, we see four ports – one for the camera, two for the robotic instrument and the fourth for the assistant’s use. Due to the high costs involved, the ideal use of robotic surgery in urology is for a partial nephrectomy in the case of cancer in the kidney, says Dr. Thilagarajah.
In other specialities this technology is used for colorectal, upper gastro-intestinal, vascular and oropharyngeal procedures, it is understood.
Robotic surgery being very hi-tech, the biggest problem for doctors who engage in these procedures is gauging how powerful this tool is. There are lots of moving parts and vision is the main thing. “You see but you don’t feel and this is the challenge that surgeons face — how much pressure should be used on the tissues, as there is no feedback except vision,” says Dr. Thilagarajah.
This is where the skill of the surgeon comes into play, it is understood. When asked when robotic surgery would become a reality in Sri Lanka, he says it won’t take that long, maybe within the next year. One robotic instrument would be adequate for the country.
With the kidney stone removal through robotic surgery not only being seen “live” in Sri Lanka but also in Sydney, Australia, and Cuibia, Brazil, he points out that it is a low-cost way of training people. On Monday, UK’s CERNO HEALTH Managing Director Gary Disley points to one suitcase and says that all the equipment needed for the live telecast is in that.
“We’ve come up with one suitcase of equipment which comprises four cameras. The other requirement is a broadband connection,” he tells the Sunday Times, explaining that the procedure is filmed, compressed and streamed on a secure private link to invited viewers.
CERNO’s website states that the Surgical Mentor System is unique in the field of surgical teaching. This system enables surgeons to communicate in real time anywhere in the world with minimal set up.


