Don’t forget to look after your brain
In 1901 a 51-year-old woman Auguste Deter was admitted to the Hospital for the Mentally Ill and Epileptics in Frankfurt, Germany. The attending physician was Dr. Alois Alzheimer. He observed Auguste over the next five years. She forgot where she had placed her things and lost her way even in her own home. She sometimes thought that people were coming to kill her. Finally she died, bedridden and incontinent.
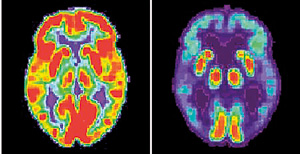
A combination image of brain scans show a normal functioning brain and one with Alzheimers.Reuters
Alzheimer autopsied her brain and identified the two hallmarks of Alzheimer’s disease, waxy protein fragments called amyloid plaques, and twisted fibres called neurofibrillary tangles. The brain disease that he identified was named after him by a colleague, Emil Kraepelin, a pioneer in psychiatry. Today the ‘A’ word has come to be feared more than the ‘C’ word. Several prominent people such as Iris Murdoch, Ronald Reagan, Charlton Heston and Margaret Thatcher have succumbed to the illness. What do we know about this illness more than a century after Alois Alzheimer described it?
The biggest risk factor for Alzheimer’s disease (AD) is age. With an increasingly ageing world population, the prevalence of AD has reached epidemic proportions. It is estimated that 40 million people worldwide suffer from the illness. It affects one in eight people aged 65 and over and 45 percent of people aged over 85.
There is no definitive treatment for AD yet, but can we take measures to reduce the chances of getting it? Memory loss is the most well-known symptom of AD but it is not the only one. There are other symptoms such as changes in personality and defects in your ability to do complex tasks. Dementia has several types but AD is the commonest. There are also other causes of brain injury other than dementia that lead to similar problems. Knowledge of such factors will help us keep our brains functioning well to old age if we do live that long. Let us look at some of these factors and then look at the possible causes of AD and other dementias.
Brain Injury
Traumatic Brain Injury (TBI) is a leading cause of disability or even death in children and adolescents. Those between the ages of 15 -24 who ride a bike, drive a motor vehicle or take part in contact sports are at high risk of brain injury. Traffic accidents account for nearly half of TBI followed by falls, assaults, suicide attempts and contact sports. TBI is significantly underdiagnosed and has no cure. Prevention is crucial and helmets, seat belts, car seats and air bags are shown to reduce the risk.
 MediScene continues our series on mental illness by Consultant Psychiatrist Prof. Raveen Hanwella. Prof. Hanwella who is attached to the National Hospital is Head, Department of Psychological Medicine, Faculty of Medicine, University of Colombo. Something bothering you? Please write in to Prof. Hanwella C/o MediScene, The Sunday Times, No. 8, Hunupitiya Cross Road, Colombo 2 or e-mail: raveensundaytimes@gmail.com MediScene continues our series on mental illness by Consultant Psychiatrist Prof. Raveen Hanwella. Prof. Hanwella who is attached to the National Hospital is Head, Department of Psychological Medicine, Faculty of Medicine, University of Colombo. Something bothering you? Please write in to Prof. Hanwella C/o MediScene, The Sunday Times, No. 8, Hunupitiya Cross Road, Colombo 2 or e-mail: raveensundaytimes@gmail.com |
After a TBI the cognitive functions might return to apparent normality but hidden damage to an area of the brain known as the frontal cortex can have serious consequences later in life. Seventy percent of damage to the brain in children is to the frontal cortex which plays a role in controlling emotions. Growth in the frontal regions of the brain continues throughout young adulthood. Blows to the head can damage the formation of insulation around nerve cells called myelin which is essential for its normal functioning. This can impair ability to control emotions leading to outbursts of anger and inappropriate behaviour. Affected children can also have difficulty in planning complex tasks and responding to social cues.
To help evaluate the seriousness of a child’s concussion after a blow to the head during sports, in the year 2000, a consensus group of medical and athletic associations developed guidelines to determine the gravity of a concussion. The guidelines divide concussion into three grades. In grade 1 concussion there is a short period of confusion, the child appears dazed without loss of consciousness. There may be inappropriate responses to easy questions. The symptoms disappear within 15 minutes. The child should be taken out of the game but if recovered after five minutes may allowed to re-join the game. But if this happens twice in a one-week period the child should wait one week before resuming any sports.
With a grade 2 concussion, the confusion can last from five minutes to an hour but there is no loss of consciousness. The child should be spoken to at five minutes intervals until the child appears normal again. The child should not re-join the game but stay away from sports for one week. If the symptoms do not disappear within a week the child should be examined by a neurologist.
With grade 3 concussion there is loss of consciousness even for a brief period of time. The child should be brought to hospital and subjected to a neurological examination. If the tests are normal and the period of unconsciousness was brief the child could go home and resume sports in one week. If the results are normal but the child was unconscious for more than a brief period the child should avoid sports for two weeks. If the nervous system examination is not normal the child should have a CAT scan or MRI scan.
The type of sports most likely to cause concussion are boxing, soccer, rugby and hockey. You should take the utmost care if you or your children are taking part in these sports. Is there a connection between repeated head injury and development of dementia including Alzheimer’s dementia in later life? In a large study looking at the risk factors for dementia called the MIRAGE study it was found that patients with AD were ten times more likely to have a history of head injury resulting in loss of consciousness and three times more likely to have a history of head injury without loss of consciousness. Further research has supported this connection. So protecting yourself from head injuries may prevent you from getting AD in later life.
Part 2 of this article will appear in our next issue



