News
Wet weather sends dengue figures up
With intermittent showers in different parts of the country sending dengue numbers up, fear is gripping men, women and children.
The dengue death toll for this year is 39 with this dreaded disease sending 10,700 people to hospitals across the country.
If a child or an adult has fever what should be done? The ‘action plan’ in such a scenario is detailed by dengue expert Dr. LakKumar Fernando who heads the Centre for Clinical Management of Dengue and Dengue Haemorrhagic Fever, Negombo.
n When someone has fever what should be done?

A ward at the Negombo Dengue Centre. Pic by Mangala Weerasekera
The most important thing is to find out as early as possible whether the fever is due to a dengue infection. Even though earlier a patient had to wait for three days before undergoing the full blood count (FBC) test to find out whether the fever was being caused by the dengue virus, now there is a test which will indicate on Day 1 of fever whether it is dengue.
If the patient is in a dengue endemic area or the country is in the throes of a dengue epidemic, it would be very important to find out whether the fever is due to dengue.
Dengue is a ‘disease of travel’. Even if someone with fever is living in a non-dengue area but has travelled to a dengue area, the first sign of dengue would be the fever. The spread of dengue is related to human travel.
n How high should the fever be to suspect dengue on Day 1?
If someone has high fever, above 100% recorded by a thermometer, then dengue should be suspected on Day 1. This should be so, even if the fever is accompanied by a cold and a cough.
n What is the test that can be done on Day 1 to detect whether it is dengue?

Dr. LakKumar Fernando
It is the Dengue NS1 Antigen Test and I have recommended to the Health Ministry that it should be made available at a controlled price.
n How effective is the Dengue NS1 Antigen Test in detecting dengue on Day 1?
It is almost 1000 effective within the first 24 hours of fever. If the fever is caused by ‘viremia’ or the virus in the blood, the Dengue NS1 Antigen Test detects the virus (antigen). If a person has high fever and it is caused by dengue, there would be a large virus load in the blood on Day 1.
After getting more than 3,000 Dengue NS1 Antigen Tests done on patients with high fever, we have found that it is 99.9% accurate in detecting dengue on Day 1 of fever. There has not been a single false negative.
n How long does it take to get the results of the Dengue NS1 Antigen Test? Where are the test kits available?
The results can be seen within half-an-hour. It’s a simple rapid testing kit which needs only a drop of blood. The test kits should be made available in pharmacies, as suggested by me to the Health Ministry. Then people will be able to buy them and go to the nearest laboratory or medical facility to get a drop of blood and check their dengue status.
n As the dengue infection progresses, how effective is the detection of dengue with the Dengue NS1 Antigen Test?
On Day 1 of fever, the detection is nearly 100%; on Day 2 it drops to 85-90%; and on Day 3 it drops to about 70% which means that when a dengue patient does the test on Day 3 of fever, there is a 30% chance of it showing a false negative. After Day 3 or 4 of fever, as the days pass, the false negativity is high. This is why it is very important to know on what day the test was done, when interpreting the results.

Ranjith De Alwis
n Why are patients not advised about the Dengue NS1 Antigen Test which can be done on Day 1 of fever itself?
Patients are in the dark because a majority in the medical community does not know how effective this test is in getting an early alarm whether it is dengue or not.
n What is the advantage of knowing on Day 1 of fever that it could be dengue?
 Generally, no patient with dengue will die within the first two days of the onset of the illness. If a patient or parents of a child know that it is dengue on Day 1, they can take stock and decide on the course of action such as which hospitals have better dengue management and go there.
Generally, no patient with dengue will die within the first two days of the onset of the illness. If a patient or parents of a child know that it is dengue on Day 1, they can take stock and decide on the course of action such as which hospitals have better dengue management and go there.
n What comes next?
On Day 3 of fever, a full blood count should be done to get an idea whether there is a reduction in the white blood cell count as well as a reduction in the platelet count. However, a full blood count could be misleading and make clinicians think it is a bacterial infection but within a few hours there could be a drastic change.
There have been cases where the platelet count was as high as 700,000 on Day 2 of fever, with a white blood cell count well above 10,000. But within two to three days, the platelet count dropped to levels as low as 5,000.
The lesson here is that even if the counts are normal on Day 2 or 3 of fever, the tests need to be repeated.
Dangerous dengue can start often when the fever settles. Usually when the fever settles, there is a sense of complacency but the patient can go into shock after that.
This is why repeating tests is essential, both in the morning and in the evening, when clinically the patient does not look good and is still feeling low, even if the fever has settled.
n What should be the ideal scenario in hospital?
When a patient’s platelet count is dropping close to 100,000, the doctors should keep a close eye for evidence of fluid leakage into the lungs or abdomen. A change in the haematocrit (percentage of the volume of whole blood made up of red blood cells) will depend on many factors – the fluid that is given to the patient; the degree of hydration or dehydration; and associations with things like bleeding.
n What is the management plan that should be followed by the doctors?
When the platelet count is 100,000 or lower, if doctors want to keep dengue deaths at zero, there are essential steps that need to be followed:
* Close monitoring of urine output every four hours. At this stage the patient should produce 1ml per kg per hour or about 150-200 ml of urine per four hours.
* Close monitoring whether there is fluid leakage inside the patient’s body by performing ultrasound scans of both the chest and the abdomen.
In many hospitals this is not followed scrupulously. Like in any disease, whatever the treatment, a majority will recover and there will be ‘records’ of ‘many successes’, hundreds in fact. But when the numbers reach the thousands, the tiny but important issue of overlooking the need to perform scans to check for leakage will invariably lead to one or two dengue deaths.
This is why the importance of scans cannot be under-estimated. Scans will help bring dengue-deaths to zero.
If when the patient’s platelet count is going down, the doctors do not check for fluid leakage through scanning, the care at that hospital is sub-optimal. Patients or their relatives need to request these scans from their doctors and if not carried out be aware that they may not be getting the best management.
n Why is it so important to check for fluid leakage in the chest or abdomen?
When the collection of fluid in the lungs or abdomen is clinically detectable, the leakage has gone on for too long. If the leaking is severe, the patient can go into shock, with the risk of death being high. If, however, the leaking is mild, even without monitoring, the patient will survive. But this just does not mean that the patient has received the best care.
n Is there a role for the media to play in reducing dengue deaths?
There certainly is. However, recent reports that ‘a spoonful of stuff’ from a veda-mahattaya or veda-hamine could have cured a little girl who had died of dengue are misleading and dangerous.
If dengue is suspected, the only place to go to is the hospital. Anyone who says that they can cure Dengue Haemorrhagic Fever (DHF) outside a hospital is making a false claim.
I challenge those who claim that they can cure DHF outside a hospital to show their skills in the Dengue Centre at Negombo. We will provide access to our DHF patients and keep the records but without interference and let them cure the DHF patients in thehospital setting. If they do that, then we will accept these claims, but not until then.m
Meanwhile, the media can educate people on dengue prevention and urge people to seek early treatment if they have fever.
| Simple measures to keep dengue at bay
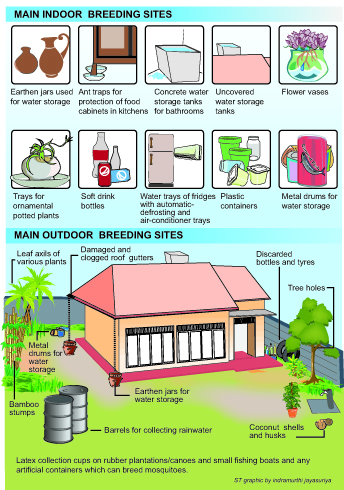
Here are some simple measures that each and every one of us can take to keep dengue at bay, according to a former Entomologist of the Dengue Control Unit, Ranjith De Alwis. n The battle against dengue should be preparedness-driven and not response-driven. It should be shared responsibility. n Knowledge about the dengue-spreading mosquitoes – Aedes aegypti and Aedes albopictus — is important. n A. aegypti is an indoor-resting mosquito, while A. albopictus is found mostly in the garden. n The female mosquitoes are highly anthropophilic (prefer human blood). They are day-biters and are around from dawn to dusk. If, however, they do not get a blood-meal during the day, they will bite at night as well. n Dengue mosquito breeding could be within homes/buildings or in the surrounding areas outside. They are mainly ‘container breeders’. (See graphic for breeding spots) n These female mosquitoes, unlike other species, do not lay a cluster of eggs directly into the water. Instead they ‘stick’ single eggs on the walls of containers having water, about ½ cm above the water-line. They prefer dark-surfaced containers, particularly red and black. Pouring out the water in such containers is not sufficient. The container-walls need to be scrubbed well to rid them of the eggs. n The eggs can survive for about one year. If the female has been infected, there could be vertical transmission, and a ‘ready-made’ dengue-infected mosquito could emerge. n The best ‘control’ method is environmental manipulation – thorough in-house checks for breeding places at least once a week or more and destroying such places. Source reduction (either elimination or reducing breeding sites) is the answer. n Don’t engage schoolchildren in cleaning-up campaigns when a dengue epidemic is on, as they would be vulnerable to being bitten by dengue-infected mosquitoes. n In hospitals, the spread of dengue could be curbed by using mosquito nets, as there could be ‘mechanical’ transmission. A female mosquito which starts biting a dengue patient could be disturbed by that patient and fly to another patient or those attending to the patients and take another bite, transferring the infection. |

