The all-important filtering organ in our body
The kidneys are a pair of amazing organs in our body, responsible for many essential tasks that keep us healthy. Each kidney, roughly the size of one’s fist is situated deep in the abdomen and consists of about a million tiny functional units called nephrons. Each nephron is a filter of its own that functions independently and overall contributes to the many functions that the kidneys are responsible for.
 The main job of the kidneys is filtration, i.e. removing toxins and excess water from the blood. Kidneys also play a vital role in controlling blood pressure. They produce a hormone named “Erythropoeitin” that trigger the production of red blood cells in the bone marrow. Kidneys are also the regulators of bone health, being the key organ that rids the body of excess calcium and phosphate, the main constituents of bones. Kidneys control the level of minerals in the blood such as sodium and potassium, the balance of which is important for good health. They are also the main regulator of the acidity in the blood getting rid of excess acid produced during metabolism in the body. The acidity indicated by a pH range (blood pH between 7.35 to 7.45) is controlled within a narrow range in our bodies to ensure proper functioning of cells. To manage this, the kidneys filter nearly 180 litres of blood daily and produce around 1.5 litres of urine concentrated with unwanted byproducts.
The main job of the kidneys is filtration, i.e. removing toxins and excess water from the blood. Kidneys also play a vital role in controlling blood pressure. They produce a hormone named “Erythropoeitin” that trigger the production of red blood cells in the bone marrow. Kidneys are also the regulators of bone health, being the key organ that rids the body of excess calcium and phosphate, the main constituents of bones. Kidneys control the level of minerals in the blood such as sodium and potassium, the balance of which is important for good health. They are also the main regulator of the acidity in the blood getting rid of excess acid produced during metabolism in the body. The acidity indicated by a pH range (blood pH between 7.35 to 7.45) is controlled within a narrow range in our bodies to ensure proper functioning of cells. To manage this, the kidneys filter nearly 180 litres of blood daily and produce around 1.5 litres of urine concentrated with unwanted byproducts.
Chronic Kidney Disease (CKD)
Progressive loss of kidney function over months or years is known as Chronic Kidney Disease (CKD ) or simply, renal failure. Many tests can detect this at a fairly advanced stage. Some test results may still be in the normal range until 50 % of the combined functions of the kidneys are lost. The disease is a progressive one where the tiny filters or the nephrons are damaged over time and start shutting down. Initially when it is only a few nephrons, the others are able to take on a greater workload and compensate for it. It is when this compensation can no longer take place that the effects are seen.
The common symptoms of CKD are fatigue, swelling of body, aches and pains, loss of appetite and nausea, itching, sleep disturbances etc. which are often disregarded as they may not be alarming initially.
Among the tests that assess kidney health, serum creatinine is the most widely used. Serum creatinine is a muscle breakdown product in the body that is used estimate kidney function. This marker starts crossing the normal range only after 50 % of kidney function is lost and therefore we now combine it with a calculation known as the estimated glomerular filtration rate (e GFR) which is a better predictor of dysfunction. Testing urine for the presence of abnormal amounts of proteins is another way of detecting kidney problems. Albumin in urine may sometimes be the earliest indication of kidney disease especially in diabetes.
CKD usually progresses slowly, and has been categorized into five stages; stage five indicating worst damage named End Stage Renal Failure (ESRF). The rate at which the disease progresses is unpredictable with some progressing very slowly over years and others in a matter of months. Often if CKD is accompanied by significant leakage of protein in the urine, it is bound to progress more rapidly.
 Burden of CKD
Burden of CKD
About 1 in 10 people have some degree of CKD. CKD can occur at any age, but it becomes more common with increasing age and is more common in women. Although about half of people aged 75 or more have some degree of CKD, many of these people do not actually have diseases of their kidneys; they have normal ageing of their kidneys. Simple blood and urine tests can detect CKD and simple, low cost treatments can slow the progression of the disease.
High blood pressure and diabetes are the leading causes of CKD. High blood pressure causes over a quarter of all cases of kidney failure. Diabetes has been established as the cause of around one-third of all cases.
Other less common conditions include inflammation (glomerulonephritis) or infections (pyelonephritis). Sometimes CKD is inherited (such as polycystic disease) or is the result of longstanding blockage of the urinary system (such as enlarged prostate or kidney stones).
Some drugs can cause CKD, especially some pain-killing drugs (analgesics) if taken over a long time. There are situations where the cause for the CKD remains undetermined.
Treating CKD
Treatment can slow the progression of CKD and prevent certain complications. The main treatments are modification of diet and medications in the early stages which would help maintain the balance normally maintained by the kidneys. When one reaches ESRF or stage 5, the options are dialysis and transplantation.
Dialysis is an artificial method of achieving the balance maintained by the kidneys by removing unwanted products and excess water from the body. However dialysis lacks some of the other functions maintained by the kidney such as the role in production of red blood cells, maintenance of mineral balance in bones and blood pressure regulation. Despite that it remains the only treatment that mimics native kidneys.
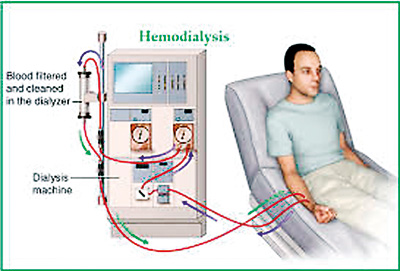
There are two main forms of dialysis: Hemodialysis is widely used in Sri Lanka and the world over. Here the patient is connected through blood lines to a machine. The blood is cleaned via the machine which has a filter made of tiny tubes similar to nephrons in the kidney. The blood is cleaned several times during a treatment session and put back into the body. To maintain a balance and have an acceptable quality of life, at least 12 hours of treatment time is required over the week. This is usually distributed over three treatment sessions each lasting four hours over the week. In Sri Lanka and many developing countries, due to lack of resources and financial constraints hemodialysis is provided mostly on a twice weekly basis, the total therapy time amounting to 8 hours a week.
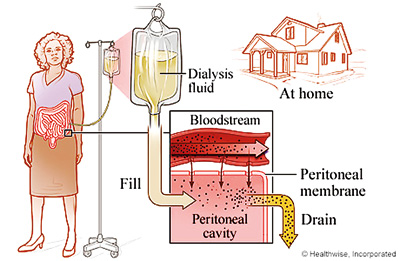
The other form of dialysis is known as Continuous Ambulatory Peritoneal Dialysis (CAPD). In this method the lining of the abdominal cavity which is called the peritoneum acts as a sieve that gets the waste products out of the body. The patient fills the abdomen with a fluid through a tube that is placed in the abdominal cavity, after which an exchange takes place between the blood vessels supplying the wall and the fluid. The fluid is removed once it is saturated with the waste products from the blood. This is a home-based therapy and the patient can even walk around and carry out his day-to-day activities while having fluid in the abdomen.
Both these forms of dialysis do not cure kidney disease but help maintain an acceptable quality of life.
Kidney Transplantation
Kidney transplantation is considered the best treatment option for most people with kidney disease. It improves the quality of life and survival is better than for those on dialysis. It is an operation where a healthy kidney is placed in a person with poorly functioning kidneys. A kidney can come from a living relative, a living unrelated person, or from a person who has died (deceased or cadaver donor). In general, organs from living donors function better and for longer periods of time than those from donors who are deceased.
Overall, transplant success rates are very good. Transplants have an 85 to 90% success rate for the first year and living donors have even better outcomes.
Preventing CKD
Early diagnosis of CKD enables certain preventive measures which have been proven successful through substantive research. Testing for kidney disease if you are considered high risk can help prevent and delay kidney disease.
Risk factors for CKD
- Hypertension
- Diabetes Mellitus
- Obesity
- Stone disease
- Recurrent urine infections
- Family history of kidney disease
- Autoimmune diseases like Systemic Lupus Erythematosus
- Certain drugs such as long term use of pain killers
- Key preventive measures are:
- Controlling blood pressure – the tighter the control within the normal range, the lesser the decline in kidney function
- Specific medications – e.g. ACE inhibitors
- Reducing salt intake to lower blood pressure
- Control of sugar and lipids
- Cessation of smoking
- Control of weight
- Increasing physical activity
( The writer is a Consultant Nephrologist, Teaching Hospital, Karapitiya, Galle)


