Don’t make the womb a tomb
View(s):
Dr. Tiran Dias
Hopes reach sky high of cuddling a beautiful baby in nine months, but a few months later there is only heartache. The shadow of stillbirth grips the couple, leaving in its wake an aching agony and the womb as a tomb. Now, hope is being held out, with Senior Lecturer in Obstetrics and Gynaecology Dr. Tiran Dias attached to the Ragama Medical Faculty showing the way on how to prevent a stillbirth. A simple, ultrasound scan when the yet-to-be born baby is about 35-36 weeks!
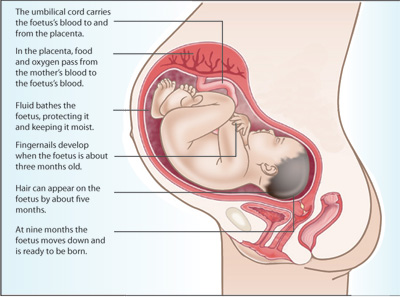
Explaining that if an expectant mother loses her baby after the 24th week of pregnancy, it is a ‘stillbirth’, Dr. Dias says that stillbirths could occur antepartum (before labour and childbirth) or intrapartum (during labour and delivery or childbirth). The full-term of a pregnancy is 40 weeks. MediScene understands that much research on this matter of life and death is ongoing between the United Kingdom and Sri Lanka.
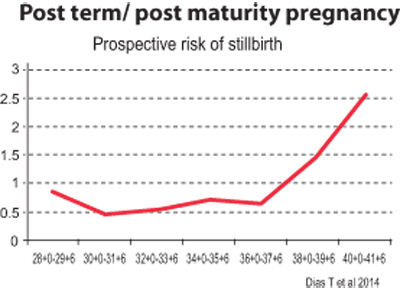
While the Colombo North (Ragama) Teaching Hospital has an ‘Obstetric Database’ detailing 6,000 antenatal mothers and the outcomes of their pregnancies, a study conducted in Ampara in 2014 has clearly indicated that the risk of stillbirth rises at 36 weeks in Sri Lankan babies and peaks at 40 weeks.
There are ‘uncontrollable’ and ‘controllable’ factors in cases of stillbirth, MediScene learns. The ‘uncontrollable’ factors include foetal deaths as a result of congenital (inherited) malformations either due to genetics or major structural abnormalities.
The ‘controllable’ factors include foetal growth restriction (FGR); maternal medical problems such as hypertension and diabetes which could cause complications in a pregnancy; or maternal infections due to viruses and protozoans, it is understood.
While a majority of stillbirths which take place antepartum are due to FGR, Dr. Dias cites recent research carried out worldwide which has made it possible to group the onset of stillbirth into two:
Stillbirths occurring before 32-34 weeks of pregnancy – under this category the danger signals of babies in trouble are easy to pick up in regular ultrasound scanning performed to check parameters.
Stillbirths occurring after 34 weeks of pregnancy – although these are in a majority, the danger signals are more difficult to catch.
Referring to why babies in difficulty after 34 weeks in the womb are hard to spot, Dr. Dias says that these babies have grown to a certain level and cannot shrink even though there may be a restriction on further growth. “Therefore, their size looks normal but the blood flow inside the baby is abnormal,” he points out.
This is when the doctors need to look closely at the unborn baby’s major arterial and venous systems and check out whether there is a Doppler blood flow abnormality. If that is missed, the end result could be a tragic intra-uterine death.
Underscoring the fact that to pick up babies at risk of term-restrictive growth, an ultrasound scan is essential at 35-36 weeks, Dr. Dias laments that because this is a new concept, no routine scans are offered at this time of pregnancy to expectant mothers in Sri Lanka.
When late onset FGR is detected, management is easy as the baby is mature and can be delivered. Usually, FGR occurs when the placenta is not adequately formed to supply the nutritional requirements of the baby in the latter part of the pregnancy.
| Preventing stillbirths Prevention of stillbirths due to foetal growth restriction (FGR) is easy, according to Dr. Dias. The measures needed are: A comprehensive risk assessment at 11-14 weeks of pregnancy which should include maternal characteristics, an ultrasound/Doppler of the blood flow in the uterine artery and maternal blood serum markers.This will help doctors predict whether a particular pregnancy is at risk not only from FGR but also pre-eclampsia. Thereafter, those at risk need to have follow-up ultrasound scans performed regularly to check out the babies’ growth from 28 weeks onwards, every three to four weekls until delivery. Dealing with intrapartum death, Dr. Dias says that each foetus is different, when taking into consideration the placental reserves it has. “As such, labour stress is not uniform in every baby. Some may show foetal heart rate abnormalities even with mild labour pains due to there being a poor placental reserve,” he points out, adding that the fundamental issue is to identify babies who are at risk at the very beginning of labour itself and offer continuous electronic foetal monitoring. Unfortunately, this is not routinely available in each and every labour room in government hospitals, MediScene learns. By performing an ultrasound scan between 11 to 14 weeks of pregnancy (the early anomaly scan), 75-80% of major structural problems can be diagnosed, with the other abnormalities being picked up at 20-22 weeks by a follow-up scan. Although termination of such a pregnancy is not an option in Sri Lanka, certain interventions at birth in the case of some congenital malformations can optimize better outcomes, adds Dr. Dias. | |


