News
Performing open brain surgery with patient an active participant
The skull is open and the brain surgeons wielding scalpels are not only slowly and steadily zeroing-in on the tumour but also its fringes.

Dr. Ruvini Abeygunaratne performing the ‘Awake Craniotomy’ flanked by Medical Officer Dr. Jeevana de Alwis Seneviratne and Scrub Nurse W.K.I. Surendra
The wonder is that 54-year-old Mallika Kumari lying on the operating table at the Lanka Hospital in Narahenpita is an active participant in the procedure.
Readily come the answers to the queries of the neurosurgical team and also responsive actions requested by them…….the names of Mallika’s daughters she gives without hesitation after which she counts from 1 to 10 and in reverse order too. Tightly she squeezes the hand of one doctor.
“Sadda ahuna, kapanawa theruna, evunata ridune ne,” laughs Mallika who lives in Anuradhapura, explaining that she heard noises in her head, felt things being cut, but there was no pain.
Four months after her open brain surgery or ‘Awake Craniotomy’, a rare surgical occurrence in Sri Lanka, Mallika stands on the threshold of the New Year with hope that she will be able to get back to her disrupted sewing business and educate her third and youngest daughter who will sit the Advanced Level examination this year.
Stressing the importance of selecting the right patient, Consultant Neurosurgeon Dr. Prasanna Gunasena points out that the ‘Awake Craniotomy’ procedure involves conscious patient–oriented progress. “The patient should be emotionally stable and not panic in the face of discomfort but rationally respond to whatever we ask her to do.”
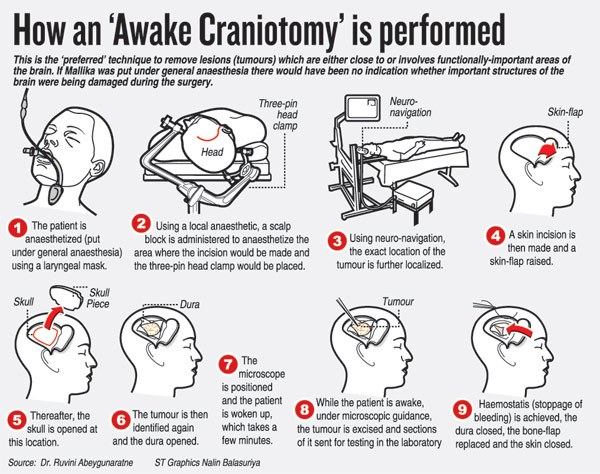
“Fascinating,” is how Consultant Neurosurgeon Dr. Ruvini Abeygunaratne describes this type of brain surgery, during which the patient is woken up half way through to check out any deficits (damage) that could be caused to the brain.

Mallika is all smiles after the ‘Awake Craniotomy’
It is not a difficult operation, according to Dr. Abeygunaratne who has done many such in the United Kingdom (UK) before she came back to Sri Lanka.
‘Awake Craniotomy’ is beneficial to the patient, as when the tumour is being taken out it is important to ensure that normal brain tissue is not damaged, causing serious repercussions.
“If the patient is unconscious, having been administered general anaesthesia, we don’t have a clue about what harm we may be causing. This changes when the patient is awake and talking.”
Recalling her experiences in the UK, she explains that when a tumour is in a sensitive region of the brain and the surgeons fear that there could be irreparable damage when excising it out, it is ‘Awake Craniotomy’ that is performed.
The importance of the Consultant Anaesthetist during such a procedure is underscored by Dr. Abeygunaratne, who explains that “a smooth wake-up of the patient” is in her able hands.
For Mallika, the mother of three daughters, the initial realisation that something was not right came soon after she and her daughters had given the first death anniversary alms-giving of her husband who himself had battled with severe illness including chronic diabetes paralysis, amputation and a massive heart attack over a 10-year period.
Suddenly during a chat with her daughters, Mallika would feel the words eluding her, the sound of her voice receding and her jaws tightening and moving in different directions. She would also drool.

Dr. Prasanna Gunasena
That was in late August and early September last year. “It passed after a minute or two,” she recalls, adding “ganang gaththe ne”. (She didn’t take much notice)
Then followed the episode when Mallika felt that unwittingly she was blinking rapidly and her vision was dimming like a “nivena bulb ekak” (flickering bulb).
At the Anuradhapura Teaching Hospital, numerous tests were carried out. It was the test using a dye which was sent to her brain indicating to the doctors that “yam deyak thiyenawa kiyala” (that there was something in her brain).
Referred to Dr. Gunasena, Magnetic Resonance Imaging (MRI) picked up what was wrong. It showed a tumour nestling in the right brain, close to a very important area that controls the power of the left arm and leg, says Dr. Gunasena, explaining that “it was not a big lesion, but a circular one about 2.5cm.
The ‘Awake Craniotomy’ was scheduled for September 17 and the neurosurgical, anaesthetic and nursing teams set to work.
By the side of Dr. Abeygunaratne, Dr. Gunasena and Medical Officer Dr. Jeevana de Alwis Seneviratne were Consultant Anaesthetist Dr. Loranthi Samarasinghe and Nurses Sriyani Thenuwara, K.A.S.C. Kuruppu, W.K.I. Surendra, G.Y.G.C.R. Jayasinghe, W.A.S.M. Wijethunge and W.M.U.J Bandara.

Dr. Ruvini Abeygunaratne
The advantages of ‘Awake Craniotomy’ are elaborated by Mallika herself. “My brain operation was done on a Thursday in Colombo and I was back home in Anuradhapura on Saturday.”
Having been advised to undergo a 30-day regimen of radiotherapy to prevent a recurrence of the tumour, Mallika has done just that at the Maharagama Cancer Hospital and now attends its monthly clinic.
“Unlike in other brain operations, in an ‘Awake Craniotomy’ we don’t insert a drain into the brain. The patient does not go into the Intensive Care Unit after surgery and the hospital stay is also reduced drastically which helps cut costs,” says Dr. Abeygunaratne, adding that Mallika went home in two days.