News
Midwives to take hypertension message to villages
 A ‘COBRA’ strike against high blood pressure, the No. 1 killer in the world, is poised for launch among the rural folk in the Puttalam district in Sri Lanka in April, under an international research collaboration made possible by a large grant from the United Kingdom (UK).
A ‘COBRA’ strike against high blood pressure, the No. 1 killer in the world, is poised for launch among the rural folk in the Puttalam district in Sri Lanka in April, under an international research collaboration made possible by a large grant from the United Kingdom (UK).
The three-year ‘Control of Blood Pressure and Risk Attenuation – Bangladesh, Pakistan and Sri Lanka’ (COBRA-BPS) trial is to be implemented with a two million sterling pound award from the UK’s Department for International Development (DFID), Medical Research Council and the Wellcome Trust.
With the goal of discovering cost-effective ways to lower high blood pressure (hypertension) among adults in South Asia, the trial will span rural areas in Sri Lanka, Bangladesh and Pakistan.
The COBRA-BPS study which will enrol 2,500 people in 30 rural communities in the three countries is led by investigators in these countries in collaboration with scientists at the Duke-National University of Singapore (NUS) Graduate Medical School and the London School of Tropical Medicine and Hygiene.
While the overall Principal Investigator is Prof. Tazeen Jafar of Duke-NUS, in Sri Lanka, the Kelaniya University’s Medical Faculty has got the privilege of conducting this crucial research which will test low-cost strategies by grassroots-level health workers and doctors to deal with hypertension.
The Sri Lankan team from the Kelaniya University’s Medical Faculty fully supported by the Health Ministry is led by Prof. Asita de Silva of the Department of Pharmacology who is also Director of the Clinical Trials Unit.
The other team members from the Medical Faculty are Senior Lecturer Dr. Channa Ranasinha and Lecturer Dr. Nathasha Luke, both from the Department of Pharmacology and Senior Lecturer Dr. Anuradhani Kasturiratne and Lecturers Dr. Manuja Perera and Dr. Dileepa Ediriweera of the Department of Public Health.
Pointing out how serious the problem of hypertension is in South Asia including Sri Lanka, Prof. Asita de Silva says that locally 1 in 5 people (20%) are a victim of this killer.
The picture gets gloomier when taking into consideration that this region is also in the throes of an epidemic of other non-communicable diseases (Nods) such as diabetes, cardiovascular diseases, chronic respiratory diseases and cancer, the Sunday Times learns.
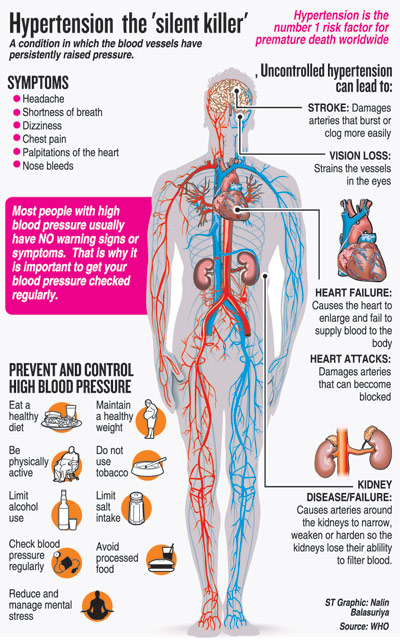
With hypertension being a major risk factor for heart attacks and stroke and also other vascular diseases which are often under-recognised leading to death and disability, Prof. de Silva underscores that lowering blood pressure seems to be the single most important way to prevent heart attacks and strokes.

Public Health Midwives undergoing training on measuring blood pressure before venturing into villages in the Kurunegala District under the pilot study concluded last year. Pix by Amila Gamage
However, even in centers of excellence in the developed world, the achievement of the target blood pressure has been possible only in 30% of patients, he says, attributing the failure to non-compliance of medical advice and not being fully aware of the disastrous consequences of hypertension.
Dr. China Ranasinha focuses on the vice-like grip hypertension has in rural areas in countries such as ours, where farmers and others who may be eking out a living as labourers would be reluctant to lose a day’s work on a visit to hospital.
This is why instead of expecting people in rural areas to come to hospital, under this trial, health workers will go to their doorstep with initial interventions to control hypertension at community level.
Commending the public health network which covers every area in Sri Lanka, Dr. Anuradhani Kasturiratne explains that the skills of Public Health Midwives (PHMs) who go to villages with the main mandate of focusing on mother and child health will be strengthened to check out hypertension in adults. The PHMs will be given extensive training and this will help in the battle against NCDs.
“High blood pressure is the leading risk factor for premature deaths globally. The findings from COBRA-BPS are likely to provide a roadmap for effective blood pressure-lowering strategies that are sustainable and can be integrated in the public health care systems in the three countries and have the potential for saving millions of lives and reducing human suffering in South Asia and possibly beyond,” says Prof. Jafar of Duke-NUS.
Sri Lanka’s Health Services Director-General Dr. Palitha Mahipala, meanwhile adds: “The Ministry of Health and its NCD Directorate support this type of high-quality community-based intervention study because if this low-cost intervention proves to be successful, it could be sustainable and scalable across the country. What is most attractive in the study design is that the interventions will be delivered through our existing primary healthcare system.”

Prof. Asita de Silva
Come April, after extensive training, armed with tools to check blood pressure, PHMs, already in place under the strong public health programme in Sri Lanka, will fan out on motorcycles to 10 remote Grama Niladhari areas in the Puttalam district.
They will each visit 100 homes, checking the pressure of every adult, says Prof. de Silva, while also spreading the message on hypertension, how changes in food habits and lifestyle including exercise could make a major difference. They will also stress he need for compliance to drug therapy, if these adults are already hypertensive.
Citing an example on how advice on nutrition would be delivered, he points out that even though the staple diet in Sri Lanka is rice, in Bangladesh rotti and in Pakistan chapathi, nutritionists at the trial centres and Duke-NUS have worked out the calorie values which the PHMs can advise rural folk to adhere to in a bid to bring down high blood pressure.
The PHMs will also refer patients with high blood pressure to the closest hospital, where the doctors would already have undergone training on the simple first-line and second-line of therapy as per national and international guidelines on controlling hypertension. Thereafter, the PHMs would keep a tab on the patients to ensure that they take their medication and go for check-ups regularly.
Is such an important but ambitious programme workable? A pilot study in Kurunegala has already been conducted last year which proves that it is workable. One thousand adults who have been detected with hypertension by PHMs have been provided with medications, while half this group, chosen randomly, has also been provided with in-depth knowledge on diet control and exercise to fight hypertension.
Have community-level low-cost interventions succeeded in lowering hypertension in rural areas? “We have to wait and see,” says Prof. de Silva, pointing out that the answer will be evident in three years when those who have been empowered with advice in addition to medication are compared to those who have not been given such advice, to check out whether their hypertension is under control.
The long-term goals of the study in Puttalam, meanwhile, are to gauge whether these low-cost interventions by health workers are scalable and sustainable. Then these interventions can be implemented not only throughout Sri Lanka but also in South Asia to prevent people from going to an early grave due to hypertension.

Dr. Channa Ranasinha
| What’s being done at a community level The interventions at community-level include:
|

