With a new lease of life it will truly be a happy b’day for this 15-year-old
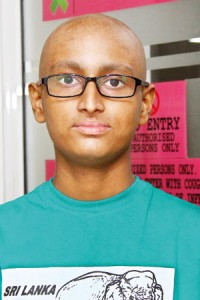
Shenon: Now he has something to celebrate about. Pix by Indika Handuwala
A lad’s life on the brink of being snuffed out by cancer……..hopes shattered into smithereens, swirling in the very depths of despair and then with the dawn of this year, a fresh lease of life.
A ‘tryst’ with tragic destiny preempted and K.M. Shenon Praminda Kumara from Kumbukgahamulla in Kuliyapitiya becomes a flag-bearer in the New Year. Smiles wreathing his face, with only a hint of a shadow behind his eyes, he is set to celebrate his 15th birthday today.
Shenon struck down by acute lymphoblastic leukaemia (ALL) is the very first in Sri Lanka to undergo an allogeneic (haplo) stem cell transplant, with only a 50% match with the donor, his father, at the state-of-the-art Bone Marrow Transplant (BMT) Unit at the Nawaloka Hospital in Colombo 2.
Having battled ALL for nearly three years, starting at the tender age of 12, and facing along with his family the highs and lows of this disease, Shenon is all smiles on Tuesday.
This pioneering transplant procedure in Sri Lanka reported to be unavailable in many other South Asian countries will not only pave the way to save numerous lives but also provide a viable option to hundreds of desperate men, women and children, who have had to seek treatment in strange foreign lands at a huge cost.
The heartbreak and agony of Shenon’s family earlier and the immense joy now, the meticulous detail with which this procedure was performed by a highly-skilled multidisciplinary medical and well-trained nursing team under the guidance of Nawaloka Hospitals’ Director-General Prof. Lal Chandrasena, we glimpse in an exclusive interview on Tuesday.
The medical team comprises Consultant Oncologist Dr. Wasantha Rathnayake; Consultant Haematologists Dr. Senani Williams & Dr. Sasikala Suresh; Consultant Physician Dr. K.D. Duminda (Coordinator of the Programme); Consultant Transfusion Physician Dr. Lakmali Morawaka; Consultant Paediatrician Dr. Deepal Perera; Consultant Microbiologist Dr. Samanmali Gunasekera; BMT Unit Coordinator Dr. Ganeshanathen Kethiswaran; and Medical Officer-in-Charge of the BMT Unit Dr. Pradeep Fernandopulle.
Before the distress of those years are put into words, the expression of Shenon’s mother, Kumudu Herath, says it all. Fevers began wracking her son’s body in 2014, says Kumudu, through the mask she is wearing to protect Shenon as she is having a cold and does not want him to catch it from her.
When he complained of severe pain in the groin area, the visits to hospitals, both private and government, and also tests and more tests began. It was at the Ragama Teaching Hospital that a bone marrow test confirmed that Shenon was afflicted with leukaemia (a cancer that affects the blood and bone marrow), she says, the day, August 20, seared into her memory.

Dr. Senani Williams
That very evening, Kumudu carried her beloved son as he could not walk through the doors of the National Cancer Institute at Maharagama, a place unfamiliar to her. Her husband, K.M. Sarath Premasiri who had served in the army was far away from home, having taken up a driving job in Saudi Arabia to keep the home fires burning.
“Shenon just couldn’t walk,” relives Kumudu, shuddering at the trauma she faced all alone that day……..“Hariyata baya hithuna,” she says, explaining that she was terrified.
Her clever son’s achievements flashed before her eyes. Always 1st in class at the Nattandiya Dhammissara National School where he was then in Grade 7, the class monitor and engrossed in books when not with his study texts.
“Jeevithe kada vatuna (life collapsed),” she sighs, adding how both she and Shenon didn’t touch a morsel of food for three days or even wash their faces.
Torn she was between her two sons when the news of the leukaemia hit her. She just could not leave Shenon alone at Maharagama for his need was greater and had to depend on the kindness of her close friend, Renuka Malkanthi Herath to look after her second son, Nirmal Shehan Nayanajith who was facing the Grade 5 Scholarship Examination.
Although she had been told not to tell Shenon about his condition, inadvertently she had left the report on his bed at Ragama while weeping over the phone to her husband. So Shenon knew what had hit him so suddenly.
“Later at Maharagama it was Dr. Wasantha Rathnayake who kept on speaking to Shenon to give him the courage and uplift his flagging spirits to come to grips with the leukaemia,” she says.
Shenon’s past agony is tangible even now as his mother recounts his illness and also his wistfulness whenever he spotted from the first-floor Ward 15A, school vans packed with laughing children whizzing past.
Her husband’s trauma was equally deep, for he needed to work to collect some money and could not be with Kumudu and Shenon facing daunting sessions of chemotherapy till April 2015. They were, however, back home for Avurudu to cook a little kiribath but the inexorable weekly clinic visits to Maharagama had become a part of their routine.
Two days he attended classes in Grade 8, she says, but there were fears of his vulnerability to catching any passing germ.
The next warning sign came with an excruciating headache in November 2015 and the heart-rending news after a bone marrow test that the leukaemia was back. Shenon’s remission (the cancer’s dormancy) was over and it was then that Sarath decided that he had to be with his beleaguered family come what may – money or no money.

Prof. Lal Chandrasena
By their side was Dr. Rathnayake, “thaththek wage”, deciding to change the medications as the cancer seemed to have affected the brain too. The new treatment, sent Shenon into severe, body-wracking bouts of vomiting.
On March 1, 2016, reluctantly while Sarath had to fly out in search of money, mother and son, headed back to Maharagama as Shenon was having fever once again, after dropping him at the airport. This time into the Intensive Care Unit he was rushed as the leukaemia was coursing through his body again.
Dr. Rathnayake’s team at Maharagama had fought hard to keep the disease
at bay.
If, however, a relapse recurred, there would be no hope. Not willing to concede defeat, Dr. Rath-nayake then offered Shenon the winning trump – “Let’s do a stem cell transplant,” by that time available at Nawaloka Hospital.
As he longs to get back to his lessons, Shenon who had sat the year-end exam of Grade 8, even though absent the whole year before that had secured above 80 marks for all subjects and a high 93 for English.
While he sets his sights on becoming a doctor, not just any doctor, but one who helps battle cancer, his parents murmur that the team members who saved their son are simply ‘Bodhi-satvas’.
| The procedure and jubilation Before delving into the medical technicalities of the allogeneic (haplo) stem cell transplant procedure, a first performed in Sri Lanka, Consultant Oncologist Dr. Wasantha Rathnayake says that Shenon came under his care for the treatment of leukaemia about three years ago. He was a very high-risk patient as along with leukaemia Shenon also had Philadelphia chromosome-positive (Ph+, a genetic abnormality). Even though all the standard protocols were carried out to fight Shenon’s leukaemia, as in the case of some with Ph+, he kept relapsing, it is learnt. With a stem cell transplant being the only option, the Nawaloka medical and nursing team, then set upon this course of treatment. “When the testing was done to get stem cells from either the father, mother or brother, there was no 100% match, which would have been the ideal,” says Dr. Rathnayake, pointing out that they also checked out the international bone-marrow donor registries. However, the father was a 50% match with Shenon’s human leukocyte antigen (HLA) tissue type and it was then that the team decided on an allogeneic (haplo) stem cell transplant. Pointing out that if the HLA match is not close enough, the donor’s immune system, which accompanies the donated stem cells, identifies the HLA mismatch and attacks the recipient’s tissues, causing graft versus host disease (GVHD), Consultant Haematologist Dr. Senani Williams says this was a major danger the team had to overcome. For those patients such as Shenon, who simply could not find an HLA-matched donor, the team seized on the fact that his father was a partial match or haplo-identical donor. While Dr. Rathnayake points out that up to the time of Shenon’s treatment using this procedure, it had only been carried out in Sri Lanka for those with thalassaemia and not leukaemia, Dr. Williams said that the ‘harvesting’ of stem cells from Shenon’s father was set for December 30, last year. It is Consultant Transfusion Physician Dr. Lakmali Morawaka who then explains the details – how Shenon’s father underwent five days of treatment by injection as an outpatient to get some of his stem cells (basic or most primitive cells which have the potential to develop into many other different types of cells) from their original location of the bone marrow to the peripheral blood circulation. “On the fifth day, a blood sample was drawn from the father to ascertain the actual number of stem-cells present to confirm whether he could be linked to the apheresis machine for the collection of his stem cells,” says Dr. Morawaka, adding that informed consent was taken from him, his health parameters checked and a central venous line fixed to his chest. Thereafter, he was connected to the apheresis machine for six hours, so that his blood flowed through the centrifuge, depositing stem cells there, while flowing back into his body. Once again, a sample of the stem cells collected in the machine was sent for testing. “There were stem cells galore,” she smiles, adding that they had collected what was required and more. Shenon, meanwhile, had been admitted to the BMT Unit 10 days before December 30, a Hickman line fixed to his chest to enable easy administration of the chemotherapy doses needed to kill off his diseased bone marrow. Then on December 30, the stem cells harvested from his father were infused to Shenon. The team waited with baited breath – for the test came 13 days later, to check whether the peripheral engraftment had taken place as well as whether the stem cells had ‘homed’ into Shenon’s bones. In two clinics miles apart, there were shouts of joy, while onlookers exchanged puzzled glances. It was Dr. Williams on the phone to Dr. Rathnayake one morning at their two different work stations – the Ragama Hospital and the Cancer Hospital.Laughter mingled with tears of joy. Later Shenon would also exhibit 100% chimerism, his own genetic cells and those of his father’s, proof that the transplant had worked. It was not just one young life saved but a vista of opportunity opened through haploidentical transplants for lots of others who are on a desperate search for donors. “There will be at least one relative who will be a 50% match for these patients. Now their stem cells can be used,” says Dr. Rathnayake holding out hope to all of them. |

Family support: Shenon with his parents and brother

Mother courage: Kumudu

Dr. Wasantha Rathnayake

Dr. Lakmali Morawaka


