It’s 3-D: Not at the movies, but in the operating theatre
View(s):Kumudini Hettiarachchi witnesses the country’s first 3-Dimensional High Definition laparoscopy or key-hole surgery in urology at work
Urology through laparoscopy is what the Sri Jayewardenepura General Hospital embarked on three years ago when others dared not go down this pathway. This year, one more notch has been upped in the technology to help this pioneering medical and nursing team to better their care and service for numerous patients who seek their help.
 The latest addition is the 3-Dimensional High Definition (3-D HD) Laparoscopy System as against the 2-D System that MediScene finds being expertly used by the team headed by Consultant Urologist and Transplant Surgeon Dr. Niroshan Seneviratne last week in the operating theatre of the semi-state Sri Jayewardenepura Hospital in Kotte. This is the first hospital in the country to own the 3-D HD Laparoscopy System for urology.
The latest addition is the 3-Dimensional High Definition (3-D HD) Laparoscopy System as against the 2-D System that MediScene finds being expertly used by the team headed by Consultant Urologist and Transplant Surgeon Dr. Niroshan Seneviratne last week in the operating theatre of the semi-state Sri Jayewardenepura Hospital in Kotte. This is the first hospital in the country to own the 3-D HD Laparoscopy System for urology.
“It is a first in laparoscopy or key-hole surgery in urology in the country,” agrees Dr. Seneviratne when asked, giving the advantages of the 3-D HD system as:
Better view of the internal area where the procedure is being performed, allowing the surgical team to get depth-perception
Greater magnification
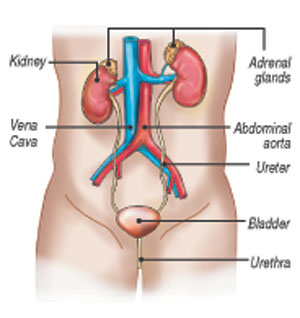
Urology is derived from the Greek ‘ouron’ (urine) and ‘-logia’ (study of) and is the branch of medicine focusing on diseases of the male and female urinary tract system and the male reproductive organs. (See graphic.) Under its purview falls genitourinary surgery, either open or laparoscopic.
As the team embarks on a nephrectomy (removal of a diseased kidney), through key-hole surgery, we too get an in-depth look at the internal organs of the patient and see what Dr. Seneviratne has been talking about.
“Here is the liver,” he says, as a sharp 3-D view of this organ fills the screen of the monitor at which he is looking and not down at the abdomen area where the minimally-invasive procedure is being performed. The diseased kidney is just below the liver, but with lots of adhesions (pasted) to most other structures in the area.
For the MediScene team, who like the surgical team performing the procedure are wearing 3-D glasses, it is like being in a cinema – with the images up-close with the feeling that one can actually touch them. The experience is “more fascinating” as Dr. Seneviratne says, for it is similar to being very much a part of the scene and remembering how when a train comes thundering in a 3-D movie, the viewers in the cinema instinctively duck.
It is a contrast from open-surgery (laparotomy), where the surgeons would be looking down, after performing a large-cut in the abdomen.
Laparoscopy is used in urology at the Sri Jayewardenepura Hospital for both kidney and prostate surgery.
Kidney surgery includes:
Nephrectomy – removal of healthy kidneys from donors for transplantation in recipients or removal of diseased kidneys either due to cancer or some other problem
Partial nephrectomy — removal of a part of the kidney which bears a cancer or tumour, preserving the uninvolved areas of the kidney
Clearing up blocks in the water pipes (ureters)
Removal of stones impacting on the kidneys
Prostate surgery – removal of the prostate due to prostate cancer

From left: Medical Officer Dr. Yasuni Manikkage;Consultant Urologist & Transplant Surgeon Dr. Niroshan Seneviratne; Main Scrub Nurse Renuka Perera; Assistant Nurse Suramya Premarathna; Orderly Neville Samarakoon; Medical Officer Dr. Chatura Hingalagoda; Theatre Technician Wijesooriya; Orderly Ananda Tissa; and Consultant Anaesthetist Dr. Chamila Pilimathalawe.
Taking up kidney operations, Dr. Seneviratne points out that usually surgery is performed on people who are ill. However, in a kidney transplant, when extracting the kidney from the donor (donor nephrectomy), the person is not ill.
So this surgery is “unique” because it is being performed on a healthy individual. As such whatever drawbacks or de-centives this healthy person would have to face should be minimized as a service to such donors, he reiterates, while also minimizing complications. “This is why we need to strive to do better. If there are no complications and the donor is up and about quickly, he/she would be more inclined to promote organ donation.”
Another very important factor is that such transplant procedures are complex surgeries.
“We have to take tissue along with lengths of crucial blood vessels, the artery and the vein, without damaging them, to implant in the recipient (the person who is receiving the kidney). We need to give him/her a good quality kidney,” explains Dr. Seneviratne, underscoring that a new life or ‘rebirth’ is being provided to that patient. These are patients who would have needed regular dialysis and finally a kidney transplant, with death staring them in the face.
Comparing the extraction of a kidney with the blood vessels intact from a donor to the delivery of a baby, he says that there needs to be absolute precision and skill because if the aorta (the main vessel providing oxygenated blood to the body from the heart) or the inferior vena cava (the main vein that carries deoxygenated blood from the lower and middle body back to the heart) get nicked or damaged, the donor would be in trouble due to haemorrhaging (bleeding).
“The 3-D HD vision now available makes such precise dissection of blood vessels easier, while the higher magnification makes us visualize the other organs better,” says Dr. Seneviratne, adding that “dissection becomes more meticulous”.
Whatever keyhole procedure is performed in urology, the 3-D HD modality helps make suturing easier as well, it is understood.
 Citing an example, Dr. Seneviratne says that if a chunk of the kidney has to be removed because of a tumour or an obstruction at the narrow pelvic-ureteric junction (PUJ) due to a congenital abnormality which manifests later in life has to be repaired, the stitching becomes easier with such vision. “Then the 2-D system is slightly more challenging, while the 3-D becomes a major boon,” says Dr. Seneviratne, pointing out that it helps in ascertaining how far to push the instruments.
Citing an example, Dr. Seneviratne says that if a chunk of the kidney has to be removed because of a tumour or an obstruction at the narrow pelvic-ureteric junction (PUJ) due to a congenital abnormality which manifests later in life has to be repaired, the stitching becomes easier with such vision. “Then the 2-D system is slightly more challenging, while the 3-D becomes a major boon,” says Dr. Seneviratne, pointing out that it helps in ascertaining how far to push the instruments.
The 3-D system obviates that limitation in suturing the structure to ensure that it remains both water-tight and blood-tight to prevent leakage of either urine or blood.
“It makes life easier for the surgeon, while for new doctors taking to this field the learning curve is quicker,” he adds.
| How laparoscopy is performed In laparoscopy or key-hole surgery which is minimally-invasive, the patient is put to sleep having been administered general anaesthesia, and three tiny cuts are made, one inside the belly-button and the other two laterally. Thereafter, a laparoscope – a medical telescope with a camera attached – is inserted into the tummy through the cut in the belly button, while gas is pumped into the stomach to expand it and also separate the organs to allow a clear vision. The camera sends pictures to a television screen and these pictures are magnified, in this case in 3-D, so that the organs are visible well. The other cuts are used for the insertion of surgical instruments.MediScene understands that unlike in laparoscopy, in a laparotomy, there is more tissue handling while exposure to air which causes drying may create adhesions (pasting). The organs inside an untouched tummy usually have a glistening, soft and slippery surface which helps them to slide over each other without friction and without attaching to each other or the abdominal wall. When such a tummy is opened up for surgery, the raw surfaces thus created result in the organs pasting not only to each other but also to the abdominal wall. In open surgery, the organ surfaces also dry up through exposure to air.However, a laparoscope helps overcome these challenges, with the gas pumped into the stomach opening up all the tissue planes and allowing the surgeon to see them highly magnified. The other advantages, of course, are minimal blood loss, less adhesions, quicker recovery, faster return to normalcy and a better cosmetic effect externally. | |


