Beware of aortic tear that could mimic a heart attack
It may not be as common in Sri Lanka as in the west but it is lethal. It can also oft be misdiagnosed as it could mimic a heart attack or even a stroke which would make it deadly for the patient, as the most common sign is excruciating chest pain. It is linked to the heart but more crucially the aorta, that foot-long tube with a diameter of more than an inch, which is the largest artery in the human body.

Dr. K. Gnanakanthan
Aortic dissection or a tear in the walls of the aorta is both lethal and deadly and commonly either detected too late or patients do not reach the hospital on time. Even if diagnosed and attended to, sadly 30% of the victims will die, MediScene learns. A clear image is created by Consultant Cardiothoracic Surgeon Dr. K. Gnanakanthan of the Kandy Teaching Hospital of what the aorta is, before he deals with what an aortic dissection is.
The aorta leaves the top of the heart’s left ventricle or muscular pumping chamber, carrying life-giving blood, through the aortic valve comprising three leaflets, to all parts of the body, he explains.
To do its duty, the aorta divides into four –
The ascending aorta, rising up from the heart, from which the coronary arteries branch off to provide blood to the heart.
The aortic arch which curves over the heart, sending out branches supplying the head, neck and arms with blood.
The descending thoracic aorta which goes down through the chest, sending smaller vessels with blood to the ribs and some chest structures.
The abdominal aorta which starts at the diaphragm and splits to form the iliac-artery pair taking blood to the lower abdomen. The branches provide blood to major organs such as the liver et al and also take blood to the legs.
Aortic dissection is all to do with the wall of the aorta, says Dr. Gnanakanthan, detailing the three thin layers of its wall.
The smooth-surfaced intima is the innermost layer allowing the easy flow of blood.
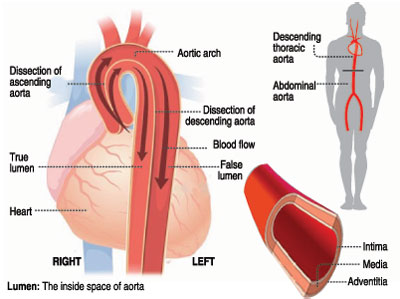 The muscle and elastic fibre containing media is the middle layer which helps to expand and contract with each heartbeat. The media is sandwiched between the innermost intima and the outermost adventitia.
The muscle and elastic fibre containing media is the middle layer which helps to expand and contract with each heartbeat. The media is sandwiched between the innermost intima and the outermost adventitia.
Providing additional support and structure to the aorta is the adventitia which is the outer layer.
An aortic dissection or tear can occur either proximally, closer to the point of the aorta’s attachment to the heart or distally, farther away from the heart, says this Cardiothoracic Surgeon who sees about 15 aortic dissections per year but lots more aortic aneurysms (a ballooning of the aorta’s walls), about 40 per year which can also be fatal if they rupture or burst.
“When such a tear or dissection takes place, blood leaks and surges within the inner intima and the middle media layers of the aorta causing the layers to separate or dissect. It may also cause a rupture or bursting of the outer-most layer which is the adventitia. If there is a rupture of the aortic wall, it would bring about instant death and the patient will not even be able to reach the hospital,” he says, underlining how serious this condition is.
The common sites of aortic dissections are the ascending aorta, the aortic arch and distal to the left sub-clavian artery arising directly off the arch of the aorta, according to Dr. Gnanakanthan.
Aortic dissections can be grouped into two:
The DeBakey classification which divides aortic dissections into Type I involving the ascending and descending aorta; Type II involving only the ascending aorta; and Type III involving only the descending aorta, after the origin of the left subclavian artery.
The Stanford classification which has Type A and includes dissections involving the ascending and the descending aorta as well as only the ascending aorta; and Type B which includes dissections involving only the descending aorta, starting after the origin of the left subclavian artery.
Explaining that in the management of aortic dissections, it is more practical to follow the Stanford classification, he says Type A, a tear in the section of the aorta where it comes out of the heart or a tear which may go down into the abdomen is more common and dangerous.
| Misdiagnosis could be fatal Reiterating the need to arrive at the right diagnosis, Dr. K. Gnanakanthan says that if an aortic dissection is misdiagnosed as a heart attack due to the ECG changes that do occur in this condition too, the treatment itself could kill the patient. “The treatment for a heart attack is blood-thinning medications and thrombolytics (blood-clot busters) when necessary. However, in an aortic dissection these would lead to massive bleeding and bring about death to the patient,” he says. | |
| Main risk factors Younger people with conditions such as Marfan Syndrome; other connective tissue disorders including Ehlers-Danlos Syndrome and Loeys-Dietz Syndrome; bicuspid aortic valve or other rarer conditions associated with weakening of the walls of the blood vessels may also be at risk, he says. Dr. Gnanakanthan says that on a smaller scale conditions such as polycystic kidney disease (PKD), an inherited disorder in which clusters of cysts develop primarily within the kidneys and annuloaortic ectasia, a dilation of the proximal ascending aorta and aortic annulus may also be contributory factors. Sudden severe chest pain as if the chest is tearing up or being ripped apart. If it is down in the descending aorta close to the iliac artery, there will be acute leg pain and numbness caused by limb ischaemia (restriction in blood supply); bowel ischaemia or kidney ischaemia. The gold standard for the diagnosis of an aortic dissection is a Computed Tomography (CT scan) aortogram where a CT scanner uses X-rays and a computer to create images of the aorta and surrounding structures. Type A (ascending and descending aorta) – will be surgically managed by the replacement of the section of the aorta which is affected, with a dacron tube. If it is a mix of Types A and B – a hybrid technique of surgery and an endovascular procedure may be used. |


