News
Fresh lease of life for many through generosity of grieving relatives
Sri Lanka marks Organ Donor Day today
Vibrant Deceased Donor Organ Donation Programme at a few state hospitals
83 very ill people get kidneys and livers in 2017
As Sri Lanka marks Organ Donor Day today, many are the men, women and children who have benefited from the Deceased Donor Organ Donation Programme in the country.

From left: Consultant Transplant Surgeon Dr. Ruwan Dissanayake, Consultant Gastroenterologist & Hepatologist Dr. Madunil Niriella, Consultant Gastroenterological, Hepatobiliary & Transplant Surgeon Dr. Rohan Siriwardana and Consultant Physician Dr. Anuradha Dassanayake. Pic by Priyantha Wickramaarachchi
A fresh lease of life has been granted to many because the next of kin of those who are declared brain-dead decided without hesitancy to donate the organs of their loved ones, while taking immense consolation that these organs have helped others to overcome death.
The laws and rules and regulations governing the Deceased Donor Organ Donation Programme are the Transplantation of Human Tissues Act of No 48 of 1987 and a detailed Circular issued by the Health Ministry in 2010. (Please see the attachments on the Sunday Times web)
Sri Lanka’s Deceased Donor Organ Donation Programme is modelled on that followed in the United Kingdom. While Sri Lanka follows an ‘opt-in’ concept, many other countries implement an ‘opt-out’ programme for deceased donor organ donation, which means that it is assumed that people will donate their organs unless they specifically ‘opt-out’, it is learnt. In Spain, where the ‘opt-out’ programme is in place, the rate of deceased donor donations is over 40 donors per million population per year.
The Sunday Times recently met an eminent medical and surgical team which has gone that extra mile to give a fighting chance for impoverished men, women and children with end-stage organ failure. They are among the poorest of the poor who seek succour from state hospitals for organs and these organs are donated to them by families, who even though overcome by grief, are ready to help others.
The team comprised Consultant Gastroenterological, Hepatobiliary & Transplant Surgeon Dr. Rohan Siriwardana; Consultant Gastroenterologist & Hepatologist Dr. Madunil Niriella; and Consultant Physician Dr. Anuradha Dassanayake of the Colombo North Teaching Hospital and Consultant Transplant Surgeon Dr. Ruwan Dissanayake of the National Hospital of Sri Lanka (NHSL).
Before getting down to organ donations, we discuss the ‘disease burden’ which creates the need for organs, with Dr. Niriella picking up the liver and Dr. Dissanayake the kidneys. Those who require these organs urgently are patients in end-stage liver disease and end-stage kidney disease and if they do not get organs in time, they face certain death.
Citing the data in Sri Lanka’s 2013 Health Bulletin, Dr. Niriella stresses that among non-communicable diseases (NCDs), even though cirrhosis is the 6th leading cause of death, it is the most-rapidly rising cause of death. There was only a 40% increase in the deaths from cardiovascular (heart) disease from 1990-2013, but with cirrhosis it was a very high 110%. This is due to a disturbing rise in non-alcoholic fatty liver disease.
Quoting in-hospital deaths, Dr. Dissanayake gives the danger figures – nearly 2,000 people die of chronic kidney disease and another 1,800 of chronic liver disease every year, notching up a tragic death toll of nearly 4,000 for these two diseases alone. These diseases are no respecters of age and anyone from a newborn to an elderly person can fall victim.
This is why there is a dire need for organs, the Sunday Times learns as Dr. Siriwardana explains that there are two types of organ donations – from live donors or from deceased (dead or cadaveric) donors.
All are categorically in agreement that the ‘best option’ is a strong Deceased Donor Organ Donation Programme, like in numerous other countries. Why is this? Taking a section of the liver from a living donor may pose a risk to the donor, is one simple answer.
The Sunday Times learns that there is no Deceased Donor Organ Donation Programme in the private sector because there is no money involved on any side – either when getting a donor or for those involved in the retrieval (harvesting) or transplant process.
The “regulated” Deceased Donor Organ Donation Programme which is of much value to the poor is in operation to a larger extent at the Colombo North Teaching Hospital; the NHSL; the National Institute for Nephrology, Dialysis and Transplantation at Maligawatte; the Sri Jayewardenepura Hospital; and the Kandy Teaching Hospital and to a smaller extent at the Anuradhapura Teaching Hospital and the Polonnaruwa Hospital.
While there were 39 deceased donors in 2017 (last year), those who have benefited by their kidneys are 72 and with their livers are 11.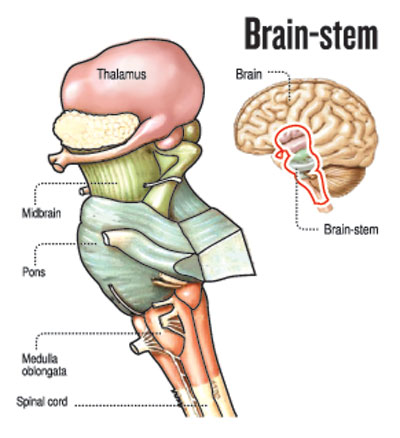
The three phases in the Deceased Donor Organ Donation Programme are explained by Dr. Dissanayake as: Phase I: In the ICU – When there is a potential brain-dead person in an Intensive Care Unit (ICU), internationally-accepted brain-dead confirmation testing is performed. The law has defined that two different doctors, with more than five years of experience, have to ‘independently and separately’ give the decision of brain-death of the patient. These two doctors would be ICU Consultants either Anaesthetists or Surgeons and Medical Officers. They are in no way linked to the Transplantation Team.
Once the two doctors independently confirm 100% brain-death, the patient is declared legally dead. Brain-death is irreversible.
It is then that the brain-dead patient’s next-of-kin is gently approached by the ICU doctors to explore the possibility of organ donation. The counselling is done by a medical doctor who is the Coordinator of the Deceased Donor Organ Donation Programme of the hospital who is trained in such counselling, after which consent is sought from the next-of-kin for organ donation. The Sunday Times understands that the next-of-kin can withdraw consent for organ donation even up to a minute before the retrieval of organs begins from the brain-dead patient.
Thereafter, the Transplantation Team is alerted about a potential transplant. Phase II: Organ donor preparation and protocols – Once the consent of the next-of-kin has been obtained, two processes take place simultaneously under this phase.
a) The preparation and maintenance of the donor for organ donation, as the organs cannot live without oxygen. As such, the brain-dead patient is kept on the ventilator to keep the lungs functioning and the heart and circulation are maintained with medications so that oxygen is delivered to the organs until retrieval takes place.
b) The legal provisions for organ donation, as many of the brain-dead patients are accident victims, are followed to the letter with the Coroner being informed and the permission of the Judicial Medical Officer (JMO) obtained.
The matching of donor and recipient (the person who is getting the organ) is also carried out by the National Blood Centre, Narahenpita. Phase III: Organ retrieval and transplantation – It is only after this that the Retrieval Team walks into the Operating Theatre and once again ticks a checklist which includes clauses whether the consent of the next-of-kin has been obtained; what the brain-dead patient’s blood group is; and whether the brain-dead patient has any unusual infections. Thereafter, the organ retrieval surgery which is complex is performed. The organs retrieved routinely are the liver, the kidneys, the lungs, the pancreas and the small bowel and tissues such as blood vessels, tendons, long bones and corneas.
During the organ retrieval operation, a special solution is infused into the organs to take out all the blood in the tissues of the organs and preserve the cells. Thereafter, the organs immersed in the special solution are transported on ice to the Transplant Centres.
Meanwhile, the potential organ-recipients are told to come to the state hospitals where they are on the register and the Transplantation Teams at these state hospitals start preparations in expectation of the organs, which are usually transported by ambulance.
Generally, the organ retrievals and transplantations are performed in the night, with doctors and nurses sacrificing precious sleep and family time, so that their other duties of looking after patients in their wards during the day have been fulfilled and they can engage in this important work undisturbed. Night-time is also conducive for the prompt delivery of the organs, without being hindered by traffic jams.
Who gets what organ is strictly decided on certain criteria. After the retrieval of organs has been carried out, according to the decision on the distribution, the organs are sent to the relevant state hospitals for transplantation.
“The organs are distributed on the basis of a scientific protocol strictly based on a priority listing of the patients awaiting organs. The severity of their disease or the most-deserving and the match between the organ and recipient are the topmost considerations,” stresses Dr. Siriwardana, while Dr. Dassanayake explains that a National Registry is needed and until such time as it is established, the state hospitals performing transplantations have their own strict list.
This list, according to Dr. Dassanayake, clearly gives all the potential recipients’ blood groups, their body sizes, the severity of their disease and life-threatening complications. So when an organ is available these are the things looked at.
| Brain-stem death and how it is confirmed | |
| There is much confusion among people about three important medical terms — coma (being comatose); persistent vegetative state and brain-death (brain-stem death). The Sunday Times spoke to Consultant Anaesthetist Dr. Bhagya Gunetilleke of the Colombo North Teaching Hospital and Consultant Intensivist Dr. Manoj Edirisooriya of the NHSL to bring about clarity on these terms and also to find out what tests are performed to make sure that a person is brain-dead.
Brain-stem death is confirmed after the determination of the absence of brain-stem function which must be due to a known cause such as major trauma like a very severe head-injury. In severe brain injury what usually happens is that the pressure within the skull rises to abnormal levels, pushing the brain and the brain stem out through an opening in the skull, which results in the cutting off of the blood supply to the brain-stem, causing its death. A massive irreversible head-injury which is not compatible with life should be confirmed through a CT scan by a Neurosurgeon. Whether the brain-stem is dead is confirmed if there is irreversible apnoea (the patient’s incapacity to breathe on his/her own). Here, through a blood test, doctors will check whether the apnoea is being caused by drugs or muscle relaxants. More tests will be performed to exclude other causes for the non-functioning of the brain stem such as very low body temperature, abnormal electrolyte (sodium/potassium) levels and certain hormone levels. After that they will perform the apnoea test to check for reversibility by allowing the carbon dioxide levels to rise, while not allowing the oxygen levels to drop. If the patient’s brain-stem is not dead, this test will prod the patient to begin breathing. There will also be cranial-nerve testing. These tests include checking the pupil and corneal reflexes, eye-ball movements, gag-reflexes and also facial responses such as grimacing to pain-stimuli to the forehead. It is after all these measures that a patient is declared brain-stem dead. A brain-stem dead person, the Sunday Times learns, even with full life-support will usually develop low blood pressure followed by multi-organ failure in 48-72 hours. |
| Who gives consent | |
| With regard to consent for organ removal from a deceased person, if he/she has not given consent before death, Section 5 of the Transplantation of Human Tissues Act states: “Relatives of any deceased person who may give consent to remove the body or any part thereof or any tissue of such deceased person. (1) On the death of any person who has not given consent for a donation effective upon death, it shall be lawful for the next of kin of such deceased person, who is above the age of twenty-one years, to give prior consent in writing for the removal of the body of such person or such part or such tissue as may be specified in such consent, for any of the purposes specified in section 2, if such deceased person had not at any time during his life expressed any contrary intention. (2) On the death of any child, it shall be lawful for both parents, or in the absence or incapacity of one parent, for the other parent, or in the absence of both parents, for the guardian of such child, to give prior consent in writing, for the removal of the body of such child or such part thereof or such tissue as may be specified in such consent for any of the purposes of section 2.” |

