News
Thyroidectomy: No major cut and quicker recovery with NOTES
Seated on a bed in Ward 7 of the National Hospital of Sri Lanka (NHSL) with a large plaster around the neck, he shyly says that it was a sip of a soft drink that he had as his first intake of fluid, while his wife chips in that she had just given him a cup of tea with some biscuits dipped in it.

Dr. Rizny Sakkaff
Unaware that he is a trailblazer, for the first-ever 3D Trans-oral Endoscopic Thyroidectomy in Sri Lanka has been performed on him, this businessman is awaiting discharge from the hospital on Friday.
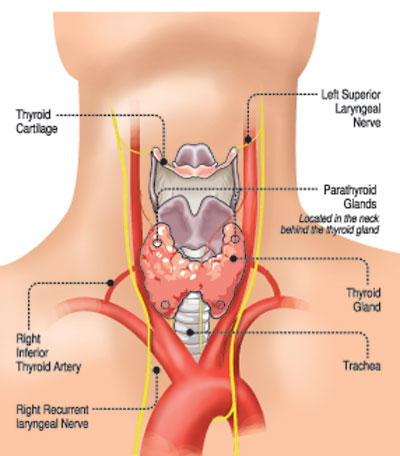
It is on Thursday that the Sunday Times meets him, armed with the information that the large plaster is just to keep the area under pressure and not to cover an external surgical cut. Usually, a thyroidectomy is the surgical removal of a part or all of the thyroid gland and entails a long cut around the lower front of the neck, leaving a scar. The butterfly-shaped thyroid gland nestles at the lower front portion of the neck internally.
The novelty of the intervention, a first in the country, performed on this patient by Consultant Ear, Nose and Throat (ENT) Surgeon Dr. Rizny Sakkaff who is also a Head and Neck Surgeon is that there are no external cuts. This procedure is not only minimally-invasive or keyhole, but also uses a ‘natural orifice’, in this case the mouth, the Sunday Times learns in an exclusive interview.
Giving the case history before delving into the procedure which is called ‘Natural Orifice Transluminal Endoscopic Surgery’ (NOTES), Dr. Rizny says that the patient had an enlarged gland. Usually, NOTES is performed on swelled glands that would be about 2-2.5cm but his was “very big” about 3.5cm. Tests indicated that it was benign, not cancerous.
Borrowing the 3D machine, which the importing company willingly provided, the 3D Trans-oral Endoscopic Thyroidectomy was scheduled for Wednesday, says Dr. Rizny who had already performed a 2D Trans-oral Endoscopic Thyroidectomy, also a first in the country, at the Kuliyapitiya Hospital in February before his transfer to the NHSL on March 1.
Wheeled into the NHSL’s Operating Theatre F, the 43-year-old patient had been put under general anaesthesia, while staff got the OT ready for this procedure.
“The placement of instruments and staff is vital,” says Dr. Rizny, pointing out that after donning the 3D glasses he took his place at the head-end of the patient and not on the patient’s side as would usually be done. The doctor assisting him was to the left of the patient, with the anaesthetist’s machine beyond him, while the assisting nurse was on the right. The 3D-monitor, giving powerful clarity to Dr. Rizny was at the leg-end of the patient.
After the usual cleaning and disinfection and the draping of the whole body, leaving exposed only the operating field, Dr. Rizny set about making three tiny cuts (incisions) inside the mouth, for the fixing of the ports. The 10mm-cut was for the endoscope with the camera which would transmit three-dimensional images to the monitor and the other two 5mm-cuts for the dissecting and coagulating instruments which he was using.
Expertly and skilfully manoeuvring the instruments through the ports while looking at the images on the monitor ahead of him, Dr. Rizny dissected the subplatysmal plane (a broad thin layer of muscle on each side of the neck), separated the strap muscles and zeroed-in on the thyroid gland. This was after identifying all the vital structures such as the trachea (breathing tube), the bunched up blood vessels and the para-thyroid, clipping them away with staples to ensure that they would not get damaged.
For, if there is damage to the laryngeal nerve there would be problems with the patient’s voice. He would also face breathing difficulties. If the para-thyroid is injured, hypoparathyroidism will be the result. This will bring about decreased blood levels of calcium (hypocalcaemia) and increased levels of blood phosphorus (hyperphosphatemia). This could cause issues like tingling in the hands, fingers and around the mouth to more severe forms of muscle cramps leading all the way to tetany or severe muscle cramping of the whole body, it is understood.

The NHSL team performing the first-ever ‘Natural Orifice Transluminal Endoscopic Surgery’ (NOTES) on Wednesday
“Hypocalcaemia is deadly because it affects the biochemistry of the patient and causes the stoppage of the heart,” says Dr. Rizny.
Thereafter, using the ‘fishtail’ (screw) movement, Dr. Rizny extricated the diseased thyroid gland and took it out. After that was the arduous task of looking at the surrounding tissue to confirm haemostasis (stoppage of bleeding).
He points out that when a patient is under general anaesthesia, the blood pressure drops but after he comes out of anaesthesia, the blood pressure can rise. Sometimes this could lull the surgeons into believing that there would be no bleeding which is a “false assumption”. This is why Dr. Rizny does the ‘valsalva manoeuvre’ (increasing intra-thoracic pressure by squeezing the ventilator bag for about 10-15 seconds) to make sure that there would be no bleeding even if the patient’s pressure rises.
Finally, as the patient had a ‘dead-space’ where the thyroid gland had been, the doctors placed an external pressure dressing to prevent blood collecting in that space. In the west, there is a special stocking made of rubber to fit under the chin, covering the neck, which will put pressure on the dead space preventing haematoma (an abnormal collection of blood outside a blood vessel) formation, it is learnt.
After the two-hour procedure, the patient was kept on the drip and fasting. Thursday morning he began his food intake with fluids.
By Friday, the patient’s bags were packed and he and his wife, full of smiles, had left the NHSL.
In the wake of this groundbreaking procedure, more patients will benefit, with the company lending the equipment for longer and Dr. Rizny hoping to schedule at least one case each on Wednesdays and Saturdays, amidst his busy theatre-list during those days.
Commending the unstinting support extended by NHSL Director Dr. Kumara Wickramasinghe, Dr. Rizny said that he provided the 5-mm stapler which was vital for the ligation of blood vessels. Referring to the essential team work which makes such a procedure a success, he paid tribute to his juniors, Dr. Mahesh Jayalath and Dr. Prageeth Gamage; Consultant Anaesthetist Dr. Ramya Amarasena, the nursing team led by Sister R.S. Janaki and the minor staff for their cooperation.

A close-up of the procedure
| Bwenefits of the procedure | |
| The benefits for the patient of the 3D Trans-oral Endoscopic Thyroidectomy when compared to open surgery include having no scar around the neck and no changes in the cosmetic appearance, quicker recovery and fewer days in hospital. Comparing the 2D and 3D systems, Dr. Rizny Sakkaff says that 2D is like sitting before the TV, while 3D is like being very much a part of the action of what is taking place on the TV. “In the 3D system, the picture quality is very good with all the structures and blood vessels clearly visible, making navigation with the instruments easier,” he says, adding that in advanced countries, robotic surgery also uses 3D technology. |

