News
Precise and speedy treatment for malignant tumours
The room plunges into darkness as the light switch is hit – but all those around the sophisticated machine, having accessed the area after walking literally through an airy maze, suddenly see green beams crisscrossing here and there.

Consultant Clinical Oncologist Dr. Shama Goonatillake explains how the sophisticated TrueBeam Radiotherapy System works. Pix by M.A. Pushpa Kumara
They are laser beams that will be used to position the patient before the TrueBeam Radiotherapy System, a first in Sri Lanka, will give out high-precision radiotherapy treatment for malignant (cancerous) tumours ranging from very small to large, with minimal harm to normal tissue surrounding them.
Friday, November 9, saw the soft opening after a pirith ceremony of the Comprehensive Cancer Care Centre of the Asiri Surgical Hospital in Narahenpita, set up in collaboration with the American Oncology Institute with its motto of ‘Precision cancer care’.
While the formal launch is today (November 18), top officials of the Asiri Group of Hospitals including Asiri Health Chief Executive Officer Dr. Manjula Karunaratne and Asiri Health Director (Operations) Dr. Samanthi de Silva and senior oncologists and Asiri Surgical staff participated in the soft opening.
The TrueBeam Radiotherapy System is unique, Dr. Karunaratne tells the Sunday Times in an exclusive interview soon after the opening, as we watch the state-of-the-art machine with its rotating gantry-head moving this way and that.
Asia including India has only a few such machines, it is learnt.
Dr. Karunaratne also points out that local specialists will have the facilities to discuss the best patient management options online with experts from the University of Pittsburg in the United States of America.
“With the TrueBeam Radiotherapy System, we can give a high dose of targeted radiation for tumour cells of all types, be they very small, as small as 0.5cm, or very large in any part of the body,” says Consultant Clinical Oncologist Dr. Shama Goonatillake based at the Comprehensive Cancer Care Centre, pointing out that it is very effective in cancer treatment.
Any type of cancer which needs radiotherapy can be treated here, it is understood.
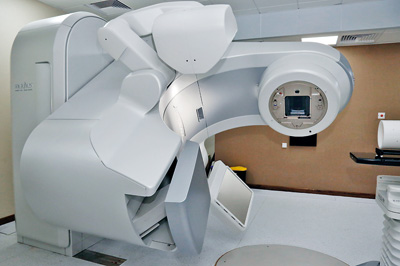
The state-of-the-art TrueBeam Radiotherapy System
Referring to the TrueBeam Radiotherapy System, Dr. Goonatillake says it is the latest model in the world and comes with a wide-range of facilities.
“This radiotherapy system is an advanced medical linear accelerator. It is fully-integrated for image-guided radiotherapy and radiosurgery and designed from the ground up to treat targets with enhanced speed and accuracy. It treats cancer anywhere in the body where radiation treatment is required including lung, breast, prostate, head and neck. Having the power not only to treat quickly, but also deliver highly precise dose rates are the system’s hallmarks,” he says, stressing that as such there is minimal damage to normal tissue surrounding the tumour cells.
The TrueBeam Radiotherapy System is complemented by the crucial CT (Computed Tomography) Simulator which will scan the cancer-affected area generating a series of images. The Radiation Oncologist will go through these images and contour the target volume treated. Then the CT Simulator will generate a 3-D (dimensional) view of the tumour, the Sunday Times learns.
Similarly, the CT Simulator can contour sensitive risk organs surrounding the tumour, says Dr. Goonatillake, pointing out that before each treatment, a verification scan would also be performed. This will be by the TrueBeam Radiotherapy System to ensure the accuracy of the therapy-targeting.
Before detailing the wide-spectrum of advanced treatment modalities available for clinicians through the TrueBeam Radiotherapy System, he explains what ‘radiation oncology’ is all about.
Radiation therapy or radiotherapy uses high-energy ionizing radiation to shrink tumours and kill cancer cells. Radiation can be delivered in two ways – external beam radiation through the use of the linear accelerator which precisely aims radiation beams from outside the body at the cancerous tumour and brachytherapy in which radioactive particles called seeds are placed within the body on the tumour or close to the cancer cells.

Dr. Manjula Karunaratne
As such, the advanced treatment modalities available through the TrueBeam Radiotherapy System (linear accelerator) will deliver external beam radiation. These modalities include:
- Intensity Modulated Radiation Therapy (IMRT) which uses advanced software to plan a precise dose of radiation based on tumour size, shape and location. The radiation is delivered using hundreds of tiny radiation beam-shaping devices known as collimators to different areas of the tumour. This spares the surrounding healthy tissue and as such has fewer side-effects.
- Rapid Arc Radiotherapy is a rotational form of IMRT but in which the daily treatment is shorter than IMRT. It is four times faster than IMRT and is better than IMRT in sparing healthy tissue.
- Image Guided Radiation Therapy (IGRT) is a radiation delivery method for tumours located in areas of the body that may change between treatment sessions due to organ filling or movements while breathing. Thus during this radiation, repeated imaging scans enable adjustment of the dosage based on any small change that may have occurred after the previous treatment.
- Stereotactic Body Radiation Therapy (SBRT) targets small isolated tumours throughout the body such as cancers in the lung or liver. Higher doses of radiation are delivered in fewer sessions.
- Stereotactic Radiosurgery is non-invasive treatment to primarily remove or wear away tumours usually in the brain. A very high dose of radiation is delivered in a single fraction, while minimizing dosage to healthy tissue. This technique is suitable for small, well-defined tumours that can be seen on a CT or MRI scan.
“Improved soft-tissue visualization via iterative Cone-Beam CT (iCBCT) provides greater visibility of soft-tissue structures and enhancements to intra-fraction motion management techniques allow clinicians to know that the cancer treatment is delivered exactly as planned,” says Dr. Goonatillake, who explains that the machine is completely digital with submillimetre accuracy and the HD MLC (high-definition multileaf collimator — 0.25cm width) will help treat even small targets.
Dr. Goonatillake takes the Sunday Times through the processes a new patient will follow when seeking treatment at the unit. The patient will be registered with his/her details, referring doctor and radiation oncologist being recorded. The patient’s history will be taken, after which he/she will be triaged, vital signs recorded and documents collected and the Consultant notified to see the patient.
The consultation will lead to a diagnosis, investigations and planning of radiotherapy, with the nursing staff being advised to scan all important documents and get PET/CT/MRI CDs in DICOM (digital imaging and communications in medicine) mode, it is learnt.
The patient and family will also have financial counselling, says Dr. Goonatillake, explaining that thereafter there will be CT simulation with the radiation oncologist, physicist, therapy radiographer and assistant in attendance. The physicist will check the images and conduct body contouring/image fusion if needed and inform the radiation oncologist about contouring, with the prescription for the radiotherapy doses being written and the physicist informed for planning. There will be many checks after that and the patient-specific plan will be drawn up.
“Before radiotherapy is delivered, we will irradiate the equipment through quality assurance. This will allow the radiation oncologist to be sure that the patient-specific plan is accurate. It is thereafter that the plan will be approved,” adds Dr. Goonatillake.

