Popping in tablets? Here’s what you should know
View(s): Most of us take medicines either for an acute illness or chronic illness.
Most of us take medicines either for an acute illness or chronic illness.
While an acute illness comes on suddenly, a chronic illness is persistent, necessitating long-term medication. Some of us also take different types of medicine.
Here, Consultant Physician Prof. Priyadarshani Galappatthy who is Professor in Pharmacology at the Department of Pharmacology, Faculty of Medicine, University of Colombo, gives us a clear and in-depth message on what we should know about those medicines we gulp down.
It is all about the safe use of medicines.
What are drugs/medicines?
A drug or a medication is a chemical or biological substance used to treat, cure, prevent or diagnose a disease or to promote well-being. It is the dose, which would determine whether it will be a ‘medicine’ or a ‘poison’.
Drugs vs medicines — why is the term ‘medicine’ preferred over ‘drugs’?
If someone says he/she is “using drugs” it would generally mean the usage of a narcotic. This is why we use the term medicine.
Why should you know about
your medicines?
Let’s take the example of a patient who has cancer. Cancer is a serious illness and as such the medicines used in its treatment are also very serious. They kill cancer cells and also normal cells. This is why there may be many side-effects when cancer medications are taken, when compared to other medicines.
Therefore, when we take medicines particularly for an illness such as cancer or another serious disease, there is only a small margin between an ‘effective’ dose and a ‘toxic’ dose.
These medicines are called ‘high-risk medicines’, since if too much is taken they can destroy too many normal cells, as in the case of a patient with cancer, which can be life threatening.
However, whether high-risk or low-risk, any medicine should be used very carefully.
What can patients do to use medicines carefully?
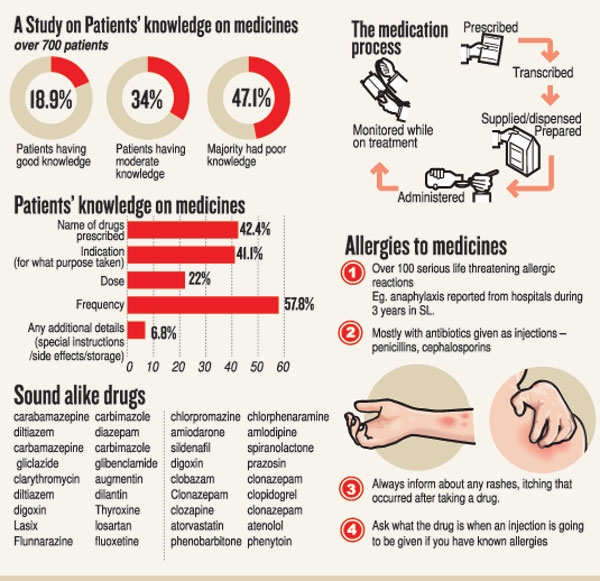
You need to know about your medicines. However, research studies have found that patients have very poor knowledge of medicines and that they do not know even minimum information about the medicines that they are taking.
What should patients know about their medicines?
There are five points of ‘essential’ minimum information that patients need to know about the medicines they are taking. (See box top right)
Here is additional knowledge that the patient should try to find out when taking medicines.
How should the medicine be stored? Are there any special storage requirements?
Some medicines need to be stored under special conditions. Eg. Insulin should be kept in the middle part of the refrigerator and not in the freezer or the fridge door.
Other medicines should be kept in bottles, which are correctly labelled.
What are the side-effects that are to be expected and are they harmful. What should you do about them?
Eg. When taking iron tablets, the person’s stools may become black – this is harmless. However, when taking pain-relieving medicines such as aspirin or ibuprofen if you have black stools that indicates bleeding into the stomach due to an ulcer and you need to stop the drug immediately and see a doctor.
What should be done if a
dangerous reaction occurs?
If a rash breaks out when taking a drug, it means that the patient is having an allergic reaction. The immediate action should be to stop the medicine and inform the doctor.
When taking anti-diabetic medicine such as insulin or glibemclamide, gliclazide, hypoglycaemia (the level of sugar in your blood dropping too low) can occur. This will result in sweating, feeling faintish or dizzy. Then what should you do? Take some sugar or something sweet.
What can happen if you do not know about your medicines?
May take a wrong dose – either too much or too little.
May not take it at the proper times.
May take it in an inappropriate manner.
The duration of taking the medicine may be incorrect.
All these are medication errors – which are common and can cause serious harm and even death.
In an article reported in the British Medical Journal in 2016, in the United States of America, medical errors are the third leading cause of death. There are 180,000 deaths per year in that country due to these errors – 51%-78% are preventable.
In another study, of about 44,000-98,000 people who die every year due to medical errors in the US, about 7,000 are due to medication errors. There are about one million preventable adverse drug reactions reportedly occurring each year in the US, costing between US$17-29 billion.
What are medication errors?
They are a failure in the treatment process that leads to or has the potential to lead to harm to the patient.
The stages in the medication process where errors can occur:
When prescribed
When transcribed (ie. When the prescribed medicine is copied into a drug chart or the dispensed label)
When supplied/dispensed
When prepared
When administered
When monitored while on treatment
Contributory factors for
medication errors
Patient factors –
Patients who are on multiple medicines
Taking high-risk medicines
Have high-risk conditions (cancers, ICU patients or psychiatric patients)
Not being knowledgeable on the medicines they are taking (poor medication literacy)
Not knowing the minimum information on medicines
Medication factors –
Some medications can be easily confused – as they ‘look alike sound alike’ (LASA); different preparations or dosages of similar medications may have similar names or packaging; and very small print on the labels, making it difficult to read them.
High-risk/alert medicines – These are associated with a high-risk of serious adverse drug events when used in error. Eg. Cancer treatment, warfarin, heparin, antibiotics, insulins and anti-diabetic medicines, pain relieving medicines such as paracetamol, ibuprofen, diclofenac sodium, opioids.
Using multiple medicines – polypharmacy. This is when a patient is taking multiple medicines, usually considered as five or more. Eg. Cancer treatment or patient has several disease conditions (Eg. diabetes, heart disease and high blood pressure in the same patient, which is not uncommon particularly in old age). There is then more room for errors and the patient needs to know about each and every medicine he/she takes and be able to identify the medicines taken for each condition (Eg. metformin for diabetes, losartan for high blood pressure and atorvastatin for cholesterol etc).
Allergies to medicines – more than 100 serious life-threatening allergic reactions (anaphylaxis) have been reported to the Adverse Reaction Reporting Centre in the Department of Pharmacology over a three-year period. These occurred mostly with antibiotics (penicillin, cephalosporin). This is why a patient needs to be vigilant and inform about rashes and itching that occur after taking a medicine. Always ask what it is, when an injection is to be given to you. If you have known allergies, you should be more vigilant.
Transitions of care – this is when patients are transferred from one location to another or come into contact with healthcare personnel. When there is a hospital admission, previously taken medicines may not be recorded; a hospital transfer; when discharged from hospital, medicines which have been revised may not be continued at home; these errors can occur even when there is an outpatient consultation or visit to a pharmacy.
Who can give information
and guide you?
The doctors treating you.
The pharmacist who dispenses your medicines
Other sources
Leaflets given on medicines.
The booklet put out by the Sri Lanka Medical Association (SLMA) available through SLMA website (www.slma.lk)
Self learning through the internet – Here you need to be careful that you are accessing authentic medical sources
Medicines information services
Eg. offered by The Department of Pharmacology, University of Colombo (0112697483), and Sri Jayewardenepura.
Other general information
to follow
Do not self-medicate for short-term illnesses. This applies specifically to antibiotics, non-steroidal anti-inflammatory drugs (NSAIDs) and steroids. These should not be taken without medical advice.
People also need to know about the commonly-used over-the-counter medicines such as paracetamol and ibuprofen.
Meanwhile, some herbal products can interact with western medicines and can cause side-effects similar to western medicines. Therefore, check with the doctor/pharmacist if you plan to take herbal products while being on western medicines.
| 5 moments of medication safety Considering the burden of medication errors globally, the World Health Organization (WHO) launched medication safety as a global challenge in 2017, with the objective of reducing serious patient harm due to medication errors by 50% in the next five years. The WHO has identified 5 moments for the patients to consider during medications to ensure safe use of medicines. The 5 moments of medication safety are: Starting a medication – the name of my medication and what is it for? The possible side-effects of my medication. Is there any other way of treating this condition? Have I informed about my allergies, other health conditions and medications? Taking my medication — How much and how often do I need to take this medication? How should I take my medication? Is there anything related to food and drinks that I need to be aware of? What should I do if I miss a dose of my medication? What should I do if I experience any side-effects? Adding a medication — Do I need another medication? If so, refer to ‘Moments 1 and 2’. Could this new medication interact with my other medications? If so, what should I do? Will I be able to manage all my medications appropriately? Reviewing my medication — Am I keeping a list of all my medications? Am I taking any medication I no longer need? How regularly should my medications be reviewed? Does my medication need any monitoring and how often should that be done? Stopping my medication — When and how should I be stopping each medication? Should any of my medication not be stopped suddenly? Have I checked if I am running out of my medications? What should I do with any remaining and/or expired medications?
| |
| Five points: ‘Minimum’ info that patients need to knowFive points of ‘minimum’ information you should know about your medicinesThe name of the medicine. Eg. Metformin.The dose that should be taken. Eg. 500mg, 750mg or 850mg. Most patients say they are taking “one tablet” but not the exact dosage they have been prescribed.For what condition is the medicine being taken? Eg. Cancer, vomiting, pain or constipation.How many times should the medicine be taken and for how long? Eg. Twice a day, 8 hourly or if needed only (Eg. when there is pain or if the patient is constipated). Is it for three days, five days, a week or long-term? Any other important information on how to take the medicine. Eg. Should the medicine be taken with food? Is it before or after a meal? If so, how long before or after? Should the patient not crush or break the tablets (Eg. this will apply in the case of slow-release tablets). |


