News
Kurunegala medical crisis – strong call for prompt probe on what is possible or not
As another week passed, the medical fraternity continued to urge the resolution of the Kurunegala Hospital controversy by holding a prompt, impartial, transparent and evidence and science-based inquiry.
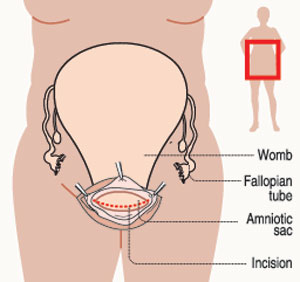
The controversy surrounds a flood of allegations of unethical sterilizations of mothers, without their consent, during Caesarean-sections (C-sections) at the Kurunegela Provincial General Hospital.
The six-member committee appointed by the Secretary of the Health Ministry visited the Kurunegala Hospital and has submitted its preliminary report, the Sunday Times learns.
This committee included two senior Consultant Obstetricians and Gynaecologists – nominated by the Sri Lanka College of Obstetricians and Gynaecologists (SLCOG) – a member from the Family Health Bureau (FHB) and several officials of the Health Ministry including investigation officers.
With some health trade unions in Kurunegala agitating in writing for a committee of inquiry to be appointed by the President, Health Ministry sources said that the Presidential Secretariat has been informed of this.
 “We are keen to continue our investigation and establish whether any alleged irregularities have occurred at Kurunegala. If any irregularities have taken place, stern action will be taken against the perpetrators,” the sources said, adding that the Director-General of Health Services has also been requested to re-send clinical protocols with regard to maternity guidelines. These strong protocols have been in place for a long time but will be sent out once again.
“We are keen to continue our investigation and establish whether any alleged irregularities have occurred at Kurunegala. If any irregularities have taken place, stern action will be taken against the perpetrators,” the sources said, adding that the Director-General of Health Services has also been requested to re-send clinical protocols with regard to maternity guidelines. These strong protocols have been in place for a long time but will be sent out once again.
The SLCOG, meanwhile, expressed “deep concern” about these reports regarding “infertility caused by intentional damage to the fallopian tubes at C-sections” and stated that “any surgical procedure performed without informed consent is unethical and unacceptable”.
Reiterating that the SLCOG has offered its technical expertise to the Health Ministry for any investigation to be done on this matter, it explained that on the request of the Health Ministry Secretary, the SLCOG nominated two members to a Panel of Investigators.
“The SLCOG would strongly urge an expeditious and transparent investigation by the authorities concerned, since the SLCOG as a professional organization does not have the authority to investigate matters of this nature,” it said.
The Sunday Times this week contacted an expert in this field to check out what is possible and what is not possible during a C-section and how fertility issues caused through an alleged unethical and unprofessional manner may be ascertained.
This follows our extensive piece last Sunday on the deep divisions within the medical fraternity; an explanation on how a C-section is performed; what tubal ligation or LRT (Ligation and Resection of the Tubes) is; and the process of obtaining consent.
The expert that the Sunday Times spoke to this week first dealt with the different techniques of suturing (stitching) the womb after the delivery of the baby in a C-section. He said there are two ways in which this may be done:
Suturing of the womb without taking it out of the abdominal incision (cut).
Suturing the womb after taking the womb out through the abdominal incision. This is called ‘exteriorization’ and some doctors do it routinely. In this case, unlike in the first technique, the fallopian tubes are easily accessible
‘Crushing’ or ‘clamping’
of tubes
Before looking into the opened up abdomen of a woman in a C-section, the expert, a Consultant Obstetrician and Gynaecologist who declined to be named said that there are no studies worldwide with regard to the alleged ‘crushing’ or ‘clamping’ of the fallopian tubes.
“So these allegations are a first in the world,” this specialist said, explaining that it was not as if the tubes had been pulled out and an injury caused.
Giving a glimpse of the ‘field of surgery’ during a C-section, he said that the abdomen is cut open along the bikini line and within this triangular opening can be seen the uterus (womb). However, the fallopian tubes cannot be seen and the doctor has to slip in his fingers along the sides and bring out the fallopian tubes, as they are on both sides of the womb.
“You have to reach in through the sides of the womb to get to the fallopian tubes,” he says, as invariably the doctor has to check the ovaries and the fallopian tubes for tumours, after the delivery of the baby and the placenta and before closing the womb and the abdomen.
However, the Consultant pointed out that this is not so in the case of ‘exteriorization’ and when conducting an inquiry into the Kurunegala issue, the Caesarian technique of the said doctor should also be evaluated.
Taking the possibilities of how the fallopian tubes may be damaged wilfully as alleged, he said that the allegations are of ‘crushing the tubes with the fingers’ or ‘clamping the tubes with forceps’.
According to this specialist:
To ‘crush’ the fallopian tubes with the fingers, the doctor will have to apply considerable force to cause injury.
To ‘clamp’ the fallopian tubes, the same would have to be done using artery forceps.
But, he explains, after the fingers are loosened or the clamp is released, the damaged area gets re-perfused (supplied with blood again). However, there are no studies or investigations to show whether the fallopian tubes can repair themselves or not. Therefore, it is very difficult to know whether an injury of this sort will lead to functional or physical damage of the fallopian tubes.
There are no histopathological studies (microscopic examination) done anywhere in the world to determine whether the crushing or clamping of the fallopian tubes has led to infertility, it is understood.
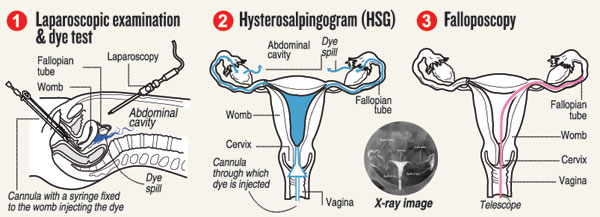
| A specialist shows the right way to determine the truth In the light of allegations being levelled about ‘crushing’ or ‘clamping’ of the fallopian tubes by a doctor at the Kurunegala Hospital, this Consultant Obstetrician and Gynaecologist recommends the following thorough inquiry to lay bare the truth once and for all. A statistical study – Pointing out that there is secondary sub-fertility in varying percentages among women who have had a first child through C-section due to adhesions etc., he says a scientific study can be carried out among the women who have been operated on by the said doctor, comparing and contrasting with a different set of women operated on by another doctor. Secondary sub-fertility has to be established clearly. A woman is deemed to have secondary sub-fertility after she has stopped breastfeeding her baby and has had unprotected coitus for 13 months. Her male partner should also not use any protection method, it is learnt. According to this Consultant Obstetrician and Gynaecologist: The first step in any investigation should be to choose the women who fit into the diagnosis of secondary sub-fertility from among those who have lodged complaints against the said Kurunegala doctor. Then this cohort of women should be matched with another cohort of women and a statistical analysis carried out. (A cohort is a group of people with a shared characteristic.) If there is a ‘significant’ statistical difference in the secondary sub-fertility rates, higher of course, in the group operated on by the said doctor, then the allegations will bear some credibility. He points out that another factor that needs to be taken into consideration is whether any of the women who have made complaints have had a definitive diagnosis of secondary sub-fertility after their previous child and whether they have independently sought treatment for this condition, before this crisis occurred at Kurunegala. “It is important to ascertain whether during this earlier treatment, a tubal patency test (to find out whether the tubes are open or unobstructed) was carried out and what the findings were. Usually, a tubal patency test will be carried out by a specialist within one year of the woman seeking treatment due to infertility issues,” he said, adding that the presence of tubal-blocks during these tests may also point towards wilful harm by the doctor who performed the previous C-section. However, when looking at the current scenario, the obvious question that arises is why until last month, no such complaints of infertility had been made by any of these women who have now come forward with these complaints. The patency of the fallopian tubes can be checked in the three following ways, says this specialist, detailing the tests: A laparoscopic examination and dye test– Laparoscopy enables a direct visual inspection of the entire external length of the fallopian tube for injury. This is a minimally-invasive (keyhole) procedure in which a fibre-optic instrument is inserted through the abdominal wall to view the fallopian tubes. Meanwhile, a dye (methylene blue) is also injected through the neck of the womb into the womb cavity. This dye will then travel along the fallopian tubes and spill out into the abdominal cavity, if the tubes are not blocked. This dye can be seen spilling into the abdominal cavity during laparoscopy, if the fallopian tubes are not blocked. Perform a hysterosalpingogram This procedure uses an X-ray to study the fallopian tubes and involves the injection of a dye which can be seen by X-ray. The dye is injected into the womb cavity through the cervix, with the use of a special cannula. The dye will then fill the womb cavity and travel along the fallopian tubes and spill into the abdominal cavity. An X-ray taken at this point will show whether there are any blocks in the fallopian tubes. Perform a falloposcopy – This is the visual examination of the inside of the fallopian tubes. A thin telescope is inserted through the neck of the womb and womb cavity to the fallopian tubes, which will show whether there is any damage to the tubes. Clincher is symmetrical “The clincher in all these examinations will be whether a woman who has been determined as having secondary sub-fertility (should fit the right definition), has symmetrical blocks of both the fallopian tubes,” says the Consultant Obstetrician and Gynaecologist, pointing out that this condition cannot be explained as being due to adhesions etc. If there are symmetrical blocks (similar blocks) in both fallopian tubes, then the answer would be clear – the doctor would have done it, adds this specialist, calling for a scientific and impartial investigation, without letting emotions get in the way. | |

