News
SL seems on a good wicket but airport closure should continue to stop re-entry of virus
Stay home and be vigilant, is the plea

Dr. Hemantha Herath
Stay home, was still the strong plea by health authorities, with cautious optimism that Sri Lanka was headed in the right direction in its efforts to stymie the spread of the new coronavirus.
“We are detecting COVID-19 patients and actively tracing all those who may have come into contact with them and quarantining them in their homes, while the lockdown continues,” said the Health Ministry’s National Coordinator for Disaster Management, Dr. Hemantha Herath, reiterating that closing down the airport was the right decision to take.
Looking at the numbers, he said the need of the hour is to be vigilant and not complacent. Sri Lanka had two peaks of confirmed cases on March 17 (when 14 cases were detected) and March 23 (when 10 cases) were detected. This Wednesday, we had ‘nil’ cases; on Thursday four confirmed cases; and Friday once again, ‘nil’ cases. This seems to put us on a better wicket than many countries such as Italy, the United States of America or the United Kingdom where there have been exponential increases in cases.
Dr. Herath believes that this is because of the strong measures taken including the closure of the airport, the lockdown, instructions on physical distancing and the stress on hand hygiene. Since the airport closure, the country has not witnessed new cases or clusters. Almost all those detected with COVID-19 have been ‘imported’ (those who have come to Sri Lanka with the virus) or ‘introduced’ (those who have been in contact with the imported cases).
“It is critical to be extra-vigilant in the next two weeks,” he urged, stressing that “we must not let down our guard until the last case is treated. Thereafter, even when we go back to normal with our work etc., we must not open the airport, as the virus is raging outside and the chances of re-entry are very high.”
If we do open the airport, there would be a massive influx of Sri Lankans from countries such as Italy where the virus has not peaked yet and there would be no keeping it at bay here, he said.
The numbers back up his argument – usually 10,000 people come in through the airport. Can we quarantine all of them? No, it is an impossible task, as already the quarantine centres are bursting at their seams. The number we did quarantine were 300-400 a day or a maximum of 500 per day, he says, adding that the total capacity of the quarantine centres does not exceed 4,000. Therefore, the answer is to keep the airport closed until the virus goes into abeyance worldwide.
Interestingly, when looking at the Epidemiology Unit’s numbers, COVID-19 confirmed cases as of Saturday morning have not been reported from the districts of Kandy, Matale, Nuwara Eliya, Hambantota, Kilinochchi, Mannar, Vavuniya, Mullaitivu, Ampara, Trincomalee, Anuradhapura, Polonnaruwa, Moneragala and Kalmunai.
The quarantine centres dotting the country are in Punani; Kandakadu; Panichchankerni; Meeyankulam; Borawewa; Galkanda; Kahagolla; Damminna; Rantembe; Diyatalawa’s Army Base Hospital and army bungalows; Gemunu Watch camp at Diyatalawa; the Light Infantry 23rd Battalion Headquarters and the Women’s Corps., both in Pampaimadu, Vauvniya; five buildings under the Security Force Headquarters in the Wanni; the Air Force’s centres in Palaly, Iranamadu and Mullaitivu; the navy’s Boossa camp; and the Hemas Club Dolphin Hotel, Negombo; John Keells’ Trinco Blu by Cinnamon; and Citrus Leisure’s Citrus Waskaduwa.
More will go home soon from NIID
A set of patients who have overcome their symptoms are awaiting discharge as soon as there is virus clearance, said Consultant Physician Dr. Eranga Narangoda, who is treating around 86 COVID-19 confirmed patients at the National Institute of Infectious Diseases (NIID).
When asked about the treatment modalities, he said that they are observed and given hydroxychloroquine, a relatively harmless drug compared to others. If the patients develop a secondary infection, an antibiotic is given.
In a clear statement, the Director-General of Health Services, Dr. Anil Jasinghe said that ‘chloroquine’ used in the treatment of malaria, will be used against COVID-19 within hospitals, specifically under medical supervision.
Do not take this drug to prevent contracting COVID-19, as the results with regard to its preventive action are negative, he said cautioning people against buying it.
Meanwhile, the National Medicines Regulatory Authority (NMRA) Director-General/CEO Dr. Kamal Jayasinghe has issued a special notification to all retail pharmacy owners that chloroquine and hydroxychloroquine should not be sold without a valid prescription.
A web search reveals that some doctors in China, South Korea and France have tested the effectiveness of this anti-malarial drug on patients and it helped block the virus from entering the cells and slowed down infections in lab cell culture, while it was ‘efficient’ in clearing the upper airways of most patients within 3-6 days.
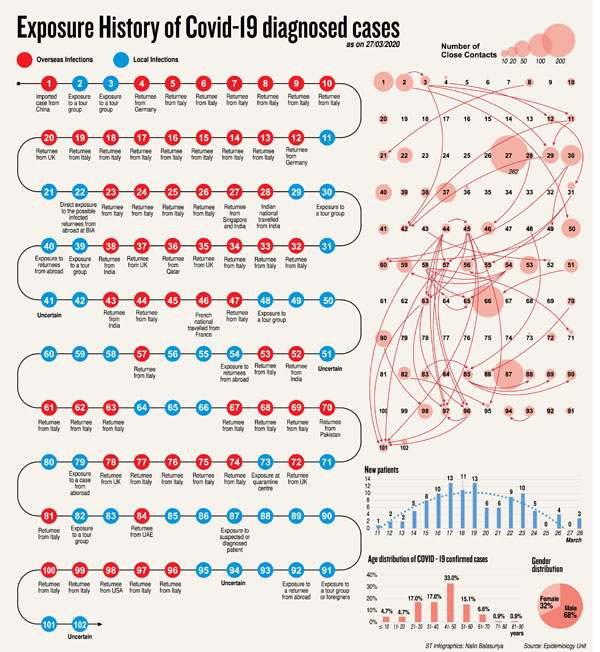
An analysis of exposure history of COVID-19 cases
Analysing the exposure history of 102 COVID-19 cases released by the Epidemiology Unit up to March 27, former Chief Epidemiologist Dr. Nihal Abeysinghe gave the following insight.
- n 100 COVID-19 cases included Sri Lankan returnees from abroad and those who contracted the COVID-19 virus locally (after excluding 1 Chinese and 1 French national)
- n Among the Sri Lankans returning from abroad: 39 ‘positive’ cases arrived from one country – Italy and 16 from the six countries of Germany, United Kingdom, United States of America, United Arab Emirates, Qatar and India
- 6 have been exposed to tour groups
- 5 directly exposed to unknown returnees
- 1 developed the disease while in a quarantine centre
- The rest numbering 33 have had close contact with some of the returnees
- 14 clusters can be identified by their inter-relations and these clusters have had 2-7 test positives; 4 clusters were connected to tour groups – the composition of which is not known; 2 clusters to returnees from India; 2 clusters to returnees from Italy; 1 cluster each to returnees from Germany, Pakistan and the United States of America; while the connection to 3 clusters is unknown
- 1,151 people have been identified as close contacts of these clusters of test positives, while 696 close contacts of those test positives but not connected to clusters are under quarantine. They are in quarantine with others who have returned from high-risk countries and as yet have not developed symptoms
Loss of smell an important symptom of COVID-19
The loss of smell without other symptoms (isolated anosmia) is an important symptom of COVID-19, states the Ear, Nose & Throat (ENT) Surgeons of Sri Lanka, citing information shared by the ENT Surgeons of the United Kingdom and the British Society of Rhinology.
These patients with isolated anosmia can increase community spread and pose a danger to medical staff, underscores the College of ENT Surgeons of Sri Lanka. “Hence, we need to include isolated anosmia as a symptom to suspect COVID-19 and to inform medical staff to take necessary precautions when handling such cases.”
The college informs the public that certain routine ENT procedures may get postponed and certain surgeries would get re-scheduled.
Take precautions against home accidents
The ENT surgeons request the public to prevent certain home accidents related to the ear, nose and throat.
- Be careful when eating or feeding children fish and meat to avoid bones getting stuck in the throat.
- Prevent the accidental insertion of foreign bodies such as toys with small parts, plastic beads, coins, hair-pins or seeds in the ear, nose or throat.
- Children should not be allowed to play with button batteries as these can cause extensive tissue damage if inserted into the ear, nose or throat.
- Children below three years of age should not be given nuts and other hard foods to eat, as these can get lodged in the airway causing an emergency.
‘It was like in a science-fiction movie’, says the very first COVID-19 Lankan patient

Dr. Eranga Narangoda
The very first Sri Lankan to be affected by the new coronavirus in the country, 52-year-old Jayantha Ranasinghe, is now back home in Mattegoda with his relieved family after 16 days (from the night of March 8 to 23) at the National Institute of Infectious Diseases (NIID), Angoda.
Thoughts and words flow easily from Jayantha as the Sunday Times has a lengthy telephone interview with him on Thursday evening as he recalls the chilling feeling that went through him on the evening of March 8, when he saw the healthcare staff in their protective gear. “It was unreal,” says Jayantha.
The events before COVID-19 were usual – from February 10-14 he took one Italian tour group and then from February 25-March 1 another. He spoke Italian as he had been in Italy for 14 long years with his wife Sujeewa, and their two children – a 20-year-old daughter and a 17-year-old son – were born there. They had returned home to Sri Lanka in the early 2000s.
Jayantha’s next duty was to pick up a group from Dickwella on March 2 and drop them off at the airport, but as it was to be early morn, he decided to go on the night of March 1 itself. Later, dropping his clients at the airport, he went home rested a little and went to the company where there was another packet with details of the next tour.
Picking up his group of four guests – two couples – on March 3, he headed for Dambulla.
“Yes, I knew about the coronavirus but was not worried as I was sure that all the checks were being done at the Katunayake airport,” he says, adding that he was prone to tonsillitis and usually wrapped a shawl around his neck against the van’s air-conditioning but forgot to do it that day.
When he reached Dambulla, his throat was sore and he had a headache and as his clients had an afternoon of leisure, he saw a doctor in the area. Next day (March 4) was the Sigiriya climb and he was feeling unfit, the sun was scorching, followed by a visit to Polonnaruwa and Habarana on the third day, all with the Dambulla hotel as the night stay.

Jayantha Ranasinghe
March 6, Jayantha drove his clients to Kandy, stopping on the way at the Dambulla temple. Even with the medicines, he was much worse. He felt as if he wanted to avva thapinna (stay in the sun) and found it difficult to stay upright. March 7 it was the Dalada Maligawa, where he showed them around with much difficulty, and on March 8 he took them to the airport.
Jayantha was very ill by that time and dropping his clients he headed home and told his wife to get a number from the doctor the family had been seeing for a long time. The doctor had told him to go immediately to the NIID…….and he was taken there by his wife in their car along with their son in the front passenger seat.
“We didn’t have the AC on and I was at the back with quite a gap between the front seats and the back seat,” he says. On reaching the NIID, the staff responded with much efficiency.
It was like in a science-fiction movie – the staff in protective gear, goggles, et al later taking him to a room on the first floor.
It was then that he felt marana biya (the fear of death) and later called his wife to tell her that it was a maaranthika rogayak (deadly disease) and if something happened to him, the family should sell his van and settle the finance payments and credit card bills.
The moment Dr. Eranga Narangoda walked in and “tak-tak gala” examined him, he knew he was in good hands.
A cough wracked his body, he couldn’t eat and he was critically ill, for in addition to the virus waging war with his body, he was also a diabetic, though it was under control.
While he got blessings and good vibes from Weerasuriya Kande Palitha Himi through the phone and many held Bodhi poojas for his recovery, he also got home-made kenda from Dr. Narangoda in addition to his medical expertise.
Now back home in Mattegoda with his family, he says his first meal was a delicious kurakkan noodles and a polos malu that his wife had lovingly prepared.
Even though the family had undergone some stress with indications that there were moves by new comers to the area to chase them away from their home, Jayantha says that the Mattegoda Police, the army and the Medical Officer of Health (MOH) and staff had been of immense support.
“They saw to all the needs of my family which was in quarantine,” says Jayantha whose ancestral home is Mattegoda, adding that he bears no ill-will towards the few people who attempted to stigmatise them.
‘Convalescent plasma’ from Jayantha for critical patient
The valuable ‘convalescent plasma’ rich with antibodies which was readily donated by Jayantha Ranasinghe who has recovered from COVID-19 was transfused to a critically ill patient on the ventilator at the NIID by Dr. Eranga Narangoda and his team yesterday to help in his recovery.
On Thursday, Jayantha had been taken to the Blood Bank of the Kalubowila Teaching Hospital for a plasma extract. “They took my consent and kept checking whether I was alright, before and after taking the blood,” says Jayantha who was at the hospital from about 9.30 a.m. to 1.30 p.m.
I was not feeling faintish or anything like that, he adds.
‘Convalescent plasma’ treatment, according to Dr. Narangoda, entails taking the blood of someone who is already infected and recovered from the coronavirus and then infusing the infection-fighting antibodies into someone who is newly-infected.
According to a study published in the ‘Lancet’ by Chinese researchers ‘convalescent plasma’ or immunoglobulins have been used to improve the survival rate of patients with SARS (Severe Acute Respiratory Syndrome), whose condition continued to deteriorate despite other treatment.


