News
Lanka’s “unique” response to battling COVID-19 in the spotlight
Sri Lanka’s “unique” strategy in combating COVID-19 came under the spotlight at the first international virtual conference on the disease ‘Breaking the transmission chain through community empowerment’.
Held by the Sri Lanka Medical Association (SLMA) and the Asia Pacific Academic Consortium of Public Health (APACPH) with an eminent panel and participants from 40 countries, the co-moderators were SLMA President & APACPH Vice President Prof. Indika Karunathilake and APACPH President Prof. Wah Yun Low from Malaysia.
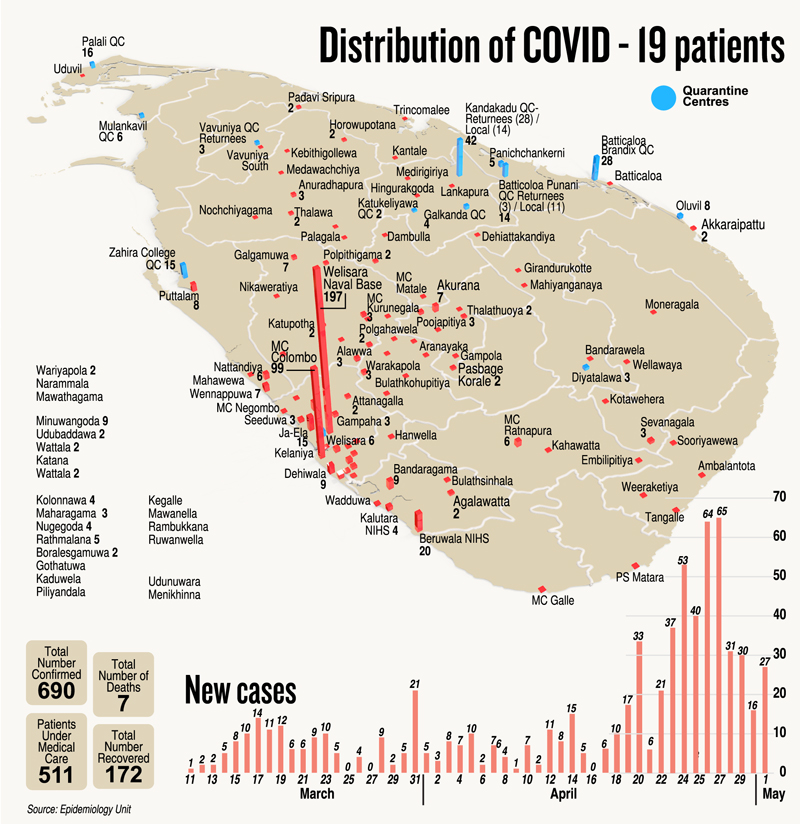
Prof. Karunathilake focused on the host country, Sri Lanka, and how it had done “exceptionally well” in controlling the situation, with the “unique” response being identification of contacts and contact tracing of high-risk individuals and quarantining them and treating them if found to be infected. This was achieved through a combined effort of the Tri-Forces, the police, law enforcement, Health Ministry and the public administrative system.
 The Head of the National Operation Centre for Prevention of COVID-19 Outbreak & Army Commander Lieutenant General Shavendra Silva said there was a need for a national strategy to underpin the coordination, collaboration and recalibration of responsibilities of different agencies for which the National Operation Centre was set up.
The Head of the National Operation Centre for Prevention of COVID-19 Outbreak & Army Commander Lieutenant General Shavendra Silva said there was a need for a national strategy to underpin the coordination, collaboration and recalibration of responsibilities of different agencies for which the National Operation Centre was set up.
As COVID-19 goes beyond a health crisis, the response was strategized into three pillars: containment of affected cases; prevention of further spreading; and minimizing the loss of life.
“The containment is spearheaded by the Tri-Forces in collaboration with the health experts; the prevention of a further spread lies in best health practices, personal responsibility and law enforcing agencies, etc; and minimizing the loss of life is handled through patient management by our great health authorities,” he said.

On the panel (from left) Dr. Ananda Wijewickrama, Prof. Indika Karunathilake, Lt. Gen. Shavendra Silva and Dr. Anil Jasinghe
Lt. Gen. Silva elaborated that containment and prevention of the spread were operationalized through the comprehensive quarantine process. Contact-tracing of the first, second and third tiers of those confirmed cases was carried out by the intelligence services of the Armed Forces and the police with the patronage of the health authorities, with PCR testing as and when required.
“With the distribution of the population in some congested areas, home-based quarantine is not possible. To negotiate this we introduced the ‘root-ball’ system, perhaps the first time in the world, in that we pulled out those who had had close contacts with confirmed cases as whole groups and transferred them to quarantine centres. The areas seemingly contaminated are designated as isolated zones, proscribing inward and outward movement,” he said.
Our approach became unique due to the ‘trinity’ of synergy, efficiency and public compliance. Synergy – experts from different fields discussed, argued and agreed upon the best response before operationalizing it and efficiency – was ensured through calibration and prioritizing of roles, responsibilities and understanding whom to support in achieving some objectives, tasks and actions to regulate the overall strategy. While elegant in its outlook, it was dependent on public compliance and came through messages sent out by the authorities through the national and private media.
The Director-General of Health Services, Dr. Anil Jasinghe, said that based on Sri Lanka’s strong public health system, the first objective was to prevent the infection coming in to Sri Lanka. But when the virus came in to the country, the next objective was to mitigate and control the infection.
“We have had at least eight recognized clusters and have been able to sort of finish off those clusters. There were two more very bad clusters especially in urban areas and sometimes linked to drug addicts etc., but even those clusters we have been able to curb, maybe 95%,” said Dr. Jasinghe.
Senior Physician from the Infectious Diseases Hospital, Dr. Ananda Wijewickrama said that at present the Health Ministry’s policy is to admit all positive cases, irrespective of their symptomatology.
“We can do that because up to now we have close to 700 patients. We have done more than 20,000 PCR tests and this number is being increased. Hospital admission, if positive, is to monitor whether they would develop symptoms and to detect any complications early and also to isolate them to curb the spread,” he said.
However, Dr. Wijewickrama cautioned that if there are more numbers, this strategy would have to be revised.
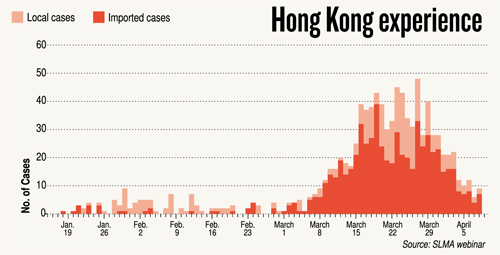
| A lesson from Hong Kong | |
 The way forward to the near-future in which the world has to live with the new coronavirus is clearly shown by SARS-buster Prof. Malik Peiris, Professor of Virology at the School of Public Health, Hong Kong University.What is next, he asks, after explaining the strong measures taken in Hong Kong, a combination of social distancing, aggressive diagnosis, contact tracing and quarantining/isolation to bring the outbreak under control. The way forward to the near-future in which the world has to live with the new coronavirus is clearly shown by SARS-buster Prof. Malik Peiris, Professor of Virology at the School of Public Health, Hong Kong University.What is next, he asks, after explaining the strong measures taken in Hong Kong, a combination of social distancing, aggressive diagnosis, contact tracing and quarantining/isolation to bring the outbreak under control. “The case numbers are very low but we cannot maintain this extent of social distancing because even though we are not in lockdown it is still hurting the economy quite dramatically. From next week Hong Kong will gradually begin to relax some of these measures. But, I think we all fully understand that this is a disease, this is a problem that will not go away,” he says. Reiterating that it is not a ‘sprint’ but a ‘marathon’, Prof. Peiris points out that the only way this outbreak will come under complete control is when the population has sufficient immunity to the virus, which means about 50% or more of the population. The only way you will get immunity is either through natural infection which will be terrible or vaccination and we know that a vaccine is still well over one year away.
Comparing the situation to being at the top of a steep hill, Prof. Peiris says that if you imagine that there is calm at the top, you still have to get to the bottom of the hill. The only way to do so is applying the brakes and releasing the brakes in a graded process so that the car doesn’t go out of control…….essentially brake hard or brake less and do this in a very informed way. “The way forward as we see it, is that Hong Kong will do some relaxation of these measures in a very gradual process but will maintain very high surveillance, very high testing and if we notice the outbreak re-emerging, then social distancing measures will be reintroduced,” he says. He too underscored the importance of contact tracing. “We now know through studies done by my colleagues at the School of Public Health that about 45% of infections are acquired before the index case develops symptoms. If a lot of transmission is taking place before the person even knows that he/she is ill, diagnosing and isolation is important but is not sufficient. You really have to get ahead of that curve and that is where the very aggressive contact tracing becomes so important.” The Hong Kong experience – the early wave starting in mid-January to end February with mainly people coming from mainland China and some local transmission. In addition to the other measures, PCR testing for diagnostics was rapidly ramped up initially, of course, focused on identifying suspected patients and their contacts and then extended to accident and emergency units and also to private practitioners. More recently, Hong Kong has also begun testing all incoming travellers at the airport, so nobody is allowed to leave the airport until they are tested and found to be negative. The second big peak (through March and early April) had come not due to people arriving from mainland China, but Hong Kong students in Europe mainly in the United Kingdom, returning home. Once again with the combination of interventions, we have been able to bring the outbreak under control, Prof. Peiris says, adding that for the last five days there has not been a single case. |


 “We have to make a long-term effort to keep this outbreak under control. So there is ‘no back to normal’ that we can think about, but we have to try to relax,” is his message.
“We have to make a long-term effort to keep this outbreak under control. So there is ‘no back to normal’ that we can think about, but we have to try to relax,” is his message.