News
Varying immune response to COVID-19: J’Pura and Oxford universities in joint study
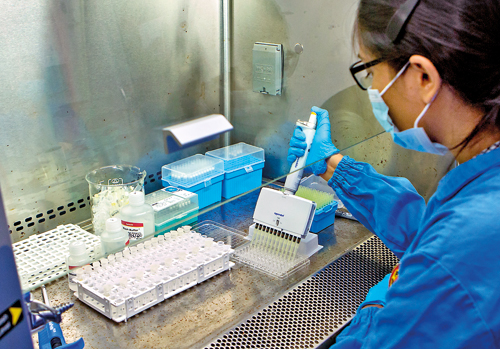
Dr. Thushali Ranasinghe plating the patient samples in a Class II safety cabinet. Pix by Sameera Weerasekera
Vital research for the betterment of humankind is what has been strengthening the bonds between two centres half-a-world between them.
On cue in keeping with the urgent needs of these troubled times and as a natural progression of the 12-year bond, these respected institutions are now looking closely to find out how the scourge of COVID-19 affects people.
These institutions are the Sri Jayewardenepura University’s Centre for Dengue Research headed by Prof. Neelika Malavige and Oxford University’s MRC Human Immunology Unit, headed by Prof. Graham Ogg, at the MRC Weatherall Institute of Molecular Medicine.
Before delving into what this immune response study would entail, Prof. Malavige says that “immunity” is the state of resistance of a person to an invading pathogen and its harmful effects. The immune response tries to prevent the development of infection and attempts to counteract, neutralize and clear the pathogen.

Dr. Thushali Ranasinghe and Dr. Deshni Jayathilaka selecting patient blood samples for the assay
The imagery she creates is simple – it is very similar to a battle or invasion and how soldiers of a country would get mobilized to ward off the threat from the invaders.
The two centres will look at how different people respond to the new coronavirus (SARS-CoV-2) which causes COVID-19.
Prof. Malavige says: “When infected with the new coronavirus, some get mild illness and recover in a week. They have mild body aches and a slight sore throat and cough. However, some others develop severe pneumonia and complications in the second week.
“Why? It is much more than to do with the virus. It is also to do with the immune response by each person to the virus. Actually if there is a detrimental immune response, there would be severe disease. As such, disease severity is not directly related to the virus but to an undesirable immune response.”

Performing the crucial PCR task to ascertain the viral loads in clinical samples is scientist Pradeep Pushpakumara
They have a hypothesis that the immune response (whether mild or severe) of a person to the new coronavirus may depend on previous exposure and illness of that person to other coronaviruses which are known to cause the common cold and upper respiratory tract infections.
“Previous exposure and infections could be a factor which may be influencing the body’s reaction to the new coronavirus, of which we know so little about. When studying the mortality figures from this virus we find that in Sri Lanka it is less than 1%, whereas in Europe and the United States of America, the case fatality rate varies between 3-9%.This is why the immune response which seems to vary needs to be studied,” she says.

Scientists of the Centre for Dengue Research meticulously going through patient samples
Understanding the immune response to the virus in a country-specific setting is crucial not only when attempting to find medications but also a vaccination against the virus, reiterates Prof. Malavige, with Prof. Ogg elaborating that by comparing immune responses from two different populations with exposure to different kinds of pathogens, “we hope to get a clearer answer about how background immunity influences COVID-19 disease”.
In the study, blood samples from the general population as well as current and recovered COVID-19 patients in the two countries would be analysed to see how T cells (a kind of white blood cell that is crucial for adapting the body’s immune response to specific pathogens), as well as antibodies (a blood protein manufactured by the body to attack specific pathogens) work in different people.
 They will compare immune markers in blood samples to get an understanding how existing immunity to different viruses (including other coronaviruses) might influence the immune response to a COVID-19 infection.
They will compare immune markers in blood samples to get an understanding how existing immunity to different viruses (including other coronaviruses) might influence the immune response to a COVID-19 infection.
“This kind of existing immunity may play a protective role or it may worsen disease severity – we just don’t know yet,” said Prof. Ogg. “By comparing immune responses from two different populations with exposure to different kinds of pathogens, we hope to get a clearer answer to this question.”
The two centres which have been engaged in strong dengue research will now expand their focus to cover the immune response not only of those who have been exposed to SARS-CoV-2 but also those who have had no such exposure.
Prof. Malavige looks at the recent past and says that Prof. Ogg, who is a Visiting Researcher at the Sri Jayewardenepura University was in Sri Lanka in February to plan this study and left just before the closure of the airport. Prof. Malavige, meanwhile, is a Visiting Researcher at Oxford University.
The immune response study has followed the essential protocols of obtaining approval from the Ethics Review Committee of the Sri Jayewardenepura University and is partnering with the National Institute of Infectious Diseases (NIID) which has treated a majority of COVID-19 patients. The British High Commission in Sri Lanka has extended Rs. 10.5 million in funding for the study.
“The Sri Lankan specimens would not be sent out of the country but studied here because we have developed our laboratory and have state-of-the-art facilities to handle complex studies,” said Prof. Malavige, adding that the specimens from British patients would be studied over at Oxford.
She adds that they will have to “work fast” and produce some results by February next year.
| Important antibody & sero-surveillance studies | |
 Dr. Chandima Jeewandara An antibody study and a sero-surveillance study have been initiated by the Centre for Dengue Research. Explaining the backdrop, Director of Operations and Clinical Services, Dr. Chandima Jeewandara says that 95% of the 4,000 diagnostic RT-PCR tests required by the Colombo Municipal Council (CMC) were carried out by them, starting with the first case of the Bandaranayake Mawatha cluster. “We responded promptly and gave the reports within 6-8 hours, enabling the CMC to trace and quarantine all close contacts, thus effectively controlling the infections and stopping their spread in Colombo city,” he said, paying tribute to Regional Epidemiologist Dr. Dinuka Guruge who was a “pillar of strength” in sending good samples, well-labelled and transported in keeping with all the guidelines. Now Dr. Jeewandara and his team have undertaken a study on the development of antibodies in blood samples being sent by the CMC. This study on around 2,000 samples of close contacts would cover the quality and quantity of antibodies. Such data would be good in deciding on a suitable vaccine when one is developed and be helpful when making clinical decisions. “We would also be able to find out whether antibody detection is linked to the person having immunity against the virus thereafter. Even though ideally it should, since this is a new virus it has not been established so far,” said Dr. Jeewandara, adding that the unit’s RT-PCR testing accuracy would also be confirmed if what they have identified as ‘positive’ brings forth an antibody positive result. Sero-surveillance on navy cluster The sero-surveillance study would cover all personnel who have been confirmed as having COVID-19 till the period ending May 30 in the navy cluster. This five-million-rupee study launched on June 1, is funded by the World Health Organization (WHO) under its ‘Unity Studies’ for sero-surveillance in an outbreak among a specific group.The aim is to understand ‘unknowns’ such as transmission pattern, severity, clinical features and risk factors for infection. Technical support including test kits are being provided under the collaboration with WHO Headquarters and Regional and Local Offices. “We are working closely with WHO’s National Professional Officer for Non-Communicable Diseases & Health Systems here, Dr. Nalika Gunawardena,” added Dr. Jeewandara.
|

