News
Born to a COVID-19 mother a little heart beats with hope after life-saving op

Dr. Sithamparanathan Mugunthan and his team carry out complex heart surgery on the two-day-old baby
A ray of sunshine and hope amidst the doom and gloom of a cyclone of COVID-19 in Sri Lanka.
A tiny newborn of a COVID-19 positive mother, just six days old, having undergone major and complicated heart surgery is now recovering in the Cardiac Intensive Care Unit (CISU) of the premier Lady Ridgeway Hospital (LRH) for Children, Colombo.
This would certainly be a first in Sri Lanka and may be even in the world, but no one has checked. For, the first and foremost duty and commitment of all those involved had been to save this fragile life.
In these troubled times of the rampaging coronavirus, this is a testament to the strength and grit of Sri Lanka’s excellent state health service and its collaborative response to give the best to the humblest of this country.
Admitted to the Avissawella Base Hospital, this COVID-19 mother (35) had given birth to twin boys, each with a birth weight of around 2.5kg, on Tuesday (May 18). Thereafter all three of them had been transferred to the Colombo East (Mulleriyawa) Base Hospital.
This was the mother’s fourth pregnancy with, sadly two miscarriages in-between, and there was much hope for the eldest child to have siblings through this pregnancy at least.
Donning the unwieldy Personal Protective Equipment (PPE), it was Mulleriyawa Hospital’s Consultant Neonatologist Dr. M.R.S.U.C Ranawaka and Consultant Paediatrician Dr. Dharshika Ranasinghe who examined the twins.
“Sensing that everything was not right with the second twin who had sub-normal levels of oxygen in his blood (low oxygen saturation), we did a chest X-ray. We also had serious concerns about the size of the baby’s heart,” says Dr. Ranawaka, explaining that the X-ray indicated plethoric lung fields.
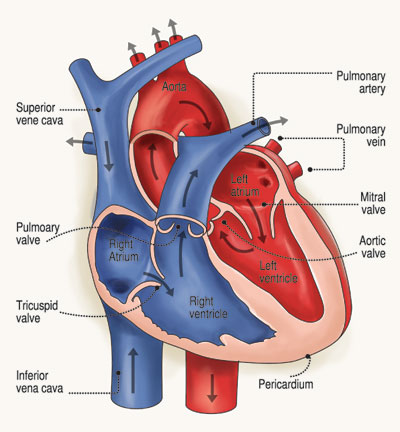 Plethoric lung fields are seen in conditions which increase the pulmonary blood flow. (Pulmonary circulation moves blood between the heart and the lungs. It transports deoxygenated blood to the lungs to absorb oxygen and release carbon dioxide. The oxygenated blood then flows back to the heart.)
Plethoric lung fields are seen in conditions which increase the pulmonary blood flow. (Pulmonary circulation moves blood between the heart and the lungs. It transports deoxygenated blood to the lungs to absorb oxygen and release carbon dioxide. The oxygenated blood then flows back to the heart.)
Dr. Ranawaka says that they had a suspicion that the baby had severe heart disease which needed to be confirmed and attended to immediately.
The super coordination between state hospitals for the benefit of this tiny patient fell into place, with him being transferred to the LRH to be seen by eminent Consultant Paediatric Cardiologist Dr. Duminda Samarasinghe without delay.
Performing an echocardiogram (an ultrasound) of the heart, Dr. Samarasinghe then confirmed that the baby had malformation in the heart called ‘Infracardiac Total Anomalous Pulmonary Venous Connection’.
“The pulmonary veins usually transfer oxygenated blood from the lungs to the left side of the heart (left atrium). But in this congenital heart anomaly (defect), instead of draining into the left atrium, the pulmonary veins form a common chamber, which drains below the diaphragm and sends the blood into the right side of the heart (right atrium) through the inferior vena cava,” explains Dr. Samarasinghe when asked by the Sunday Times.
The baby needed emergency surgery and an immediate and intense discussion on logistics ensued among the different specialities on how to give the little patient critical post-surgical care as LRH was not a COVID-19 treatment hospital, while not jeopardizing the other patients already in the ICU.
All wheels, though heavy and involving much work, have turned smoothly, with the LRH’s multidisciplinary staff rising to the occasion. They included the Paediatric Cardiology Team guided by Dr. Duminda Samarasinghe; the Cardiac Surgical Team by Consultant Cardiothoracic Surgeon Dr. Sithamparanathan Mugunthan; the Cardiac Anaesthesia Team by Consultant Cardiac Anaesthetist Dr. Thusitha Jayathilaka; and the Cardiac Intensive Care Team by Consultant Paediatric Cardiac Intensivist Dr. Manjula Hewageegana and their nursing teams.
An ICU is a busy place with most patients being attached to ventilators and the work that would have gone into moving other little ones to isolate this baby would have been tremendous, says Mulleriyawa Hospital’s Dr. Ranawaka, adding simply that the state health sector “patients-lava atha arinne ne (won’t abandon patients)”.
| It was a matter of life and death“It was a dire emergency – this Obstructed-Infracardiac Total Anomalous Pulmonary Venous Connection was a matter of life and death,” says Consultant Cardiothoracic Surgeon Dr. Sithamparanathan Mugunthan. Taking all precautions including wearing the hot and heavy PPE against COVID-19, as the baby’s mother had earlier tested positive, Dr. Mugunthan and his team set about repairing the heart defect of the two-day-old baby boy before them on the operating theatre table on Wednesday (May 19). Imagine, how tiny the baby’s heart is…….unfazed they set about the complicated open heart surgery lasting nearly eight hours from 9 p.m. on Wednesday (May 19) to around 3.30 a.m. on Thursday (May 20). While Consultant Cardiac Anaesthetist Dr. Thusitha Jayathilaka and his team; Perfusionists Rohitha Thilakaratne and Anoma Kandanarachchi; and the Nursing Team under the guidance of M.G. Shamintha Nirmalee were invaluable members who gave of their all for the surgery, the health assistants had also been very active during the procedure.
| |
| A happy family with 2 newcomersOverjoyed is Shamal Harindra Gnanaratne and his elder daughter who is 10 years old.Not one but two new members have just become a part of the family, with the twin-boys being born on Tuesday (May 18). Shamal, a policeman attached to Police Headquarters, although in quarantine back home in Ruanwella, is longing for the day when he can see his wife and hold his newborn sons close. “Wifta avulak ne, amaruwak ne,” he says, adding that his wife is okay. |

