Have I got Cervical Cancer?A good prevention programme including the use of home remedies to detect it, could help keep this second most common cancer in Sri Lanka among women at bay. The picture on the screen was of an elephant - a huge one at that, at the presentation at the Family Health Bureau auditorium.
Around 230,000 women die of cervical cancer each year. In Sri Lanka, there are around 1,100 new cervical cancer cases per year and this is the second largest killer among cancers that affect women, the first being breast cancer. What is the answer? The obvious one is early diagnosis through a pap smear, and then treatment. But Prof. Paul D. Blumenthal of the Johns Hopkins University had a different view on the development and adoption of appropriate strategies for cervical cancer prevention in low-income settings, the important word being appropriate. Take some of the Sri Lankan settings - yes, we have a commendably low infant and maternal mortality rate and also a health system that reaches out through a network of family health workers to every village. However, can all women in the crisis age-group get themselves tested through pap smears, for which they have to come to a clinic? Even if they do get themselves tested and are found to be positive, how many will come for follow-up treatment crucial to keep this killer at bay? With families to look after, water to carry, fields to work, hardly a bus plying through villages in the remoter areas, some women may come for follow-up treatment when it is too late. Their solution could lie in a simple test that can be carried out in the homes of the women themselves by the family health worker, using what every kitchen has.
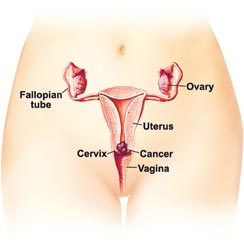
"Vinegar," explains Prof. Blumenthal stressing that cervical cancer is preventable when pre-cursor lesions are detected and treated before they develop into cancer. Pointing out a unique public health opportunity, he says that what is needed is just two weeks of training for the family health worker. "Visual inspection with acetic acid (VIA) involves only swabbing the cervix with a 3-5% acetic acid (vinegar) solution before examination using a strong light such as a good torch," says Prof. Blumenthal adding that sensitivity to VIA is equivalent to or better than that of cytologic examination. The vinegar would turn abnormal cells white indicating malignancy and the health worker only needs her eyes to spot it. With women in remote areas, the barrier is follow-up care. They have to get a pap smear done, then a colposcopic examination or biopsy and then come again for treatment, he said adding that along with the VIA or Lugol's iodine test, the health worker could treat the woman immediately if she is armed with the cryo-gun to administer cryotherapy. MediScene learns that cryotherapy is the application of extreme cold to destroy diseased tissue. Prof. Blumenthal details a good prevention programme as being able to reach a significant percentage of at-risk women; including effective testing; treating and managing women who test positive, ensuring effective follow-up and monitoring and evaluation. Cervical cytology has limitations because for that not only laboratories but also cyto-technicians are needed, according to him. "VIA, however, is technology that works in unsophisticated surroundings while also being inexpensive. All test requirements are materials available locally and the tests can be performed by non-physicians." Which one is cheaper? Which one gives immediate results? VIA and cryotherapy seem to be the obvious answers. "Once covered, the women don't need to come to the clinic for five years. One screening reduces death by 30%," he says, whereas if a woman is tested positive in a pap smear but doesn't come back it is a missed opportunity to save a life. The “good” is not the enemy of the “best”, he says. The best is the pap smear but what if you can't do it? Then acetic acid or iodine will be as good, is the important message from Prof. Blumenthal.
|
|| Front
Page | News | Editorial | Columns | Sports | Plus | Financial
Times | International | Mirror | TV
Times | Funday
Times | Medi Scene || |
| |
Copyright
2007 Wijeya
Newspapers Ltd.Colombo. Sri Lanka. |