News
Dangers of super-bugs ‘Urgent need to halt abuse and misuse of antibiotics’
View(s):By Kumudini Hettiarachchi
This is why World Antimicrobial Awareness Week from November 18-24 is of utmost importance. It is all about fighting ‘super-bugs’, says Consultant Clinical Microbiologist Dr. Madhumanee Abeywardena attached to the Kandy National Hospital. She also represents the Sri Lanka College of Microbiologists.
The World Health Organization (WHO) reiterates that Anti-Microbial Resistance (AMR) threatens the effective prevention and treatment of an ever-increasing range of infections caused by bacteria, parasites, viruses and fungi.
AMR occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines, making infections harder to treat and increasing the risk of disease spread, severe illness and death. As a result, the medicines become ineffective and infections persist in a person’s body, increasing the risk of spread to others.
Anti-microbials – including antibiotics, antivirals, antifungals and antiparasitics – are medicines used to prevent and treat infections in humans, animals and plants. Micro-organisms that develop anti-microbial resistance are sometimes referred to as “superbugs”.
Dr. Abeywardena goes back to the urine infection to explain that we may consider it to be a “simple” infection. The automatic assumption would be that the doctor would give some medication and everything would be fine. If there is fever, the doctor will order a urine culture, while prescribing an antibiotic. The patient scrupulously takes the antibiotics while awaiting the culture report but there is no sign of an improvement in the condition.
Why?
“This is because if it is Klebsiella pneumoniae, it is a bacterium resistant to antibiotics. This resistant bacterium will get into the bloodstream through the kidneys and go everywhere in the body in huge numbers. Even though hospital staff will do their utmost, the patient will die as there is no antibiotic that can kill this particular bacterial population! It is similar to the gloomy period before antibiotics were discovered – the pre-antibiotic era,” says Dr. Abeywardena.
She points out that this scenario is taking place in many hospitals all over the world, mainly in Asia and Africa, not only with regard to Klebsiella pneumoniae but also several more resistant micro-organisms.

Dr. Madhumanee Abeywardena
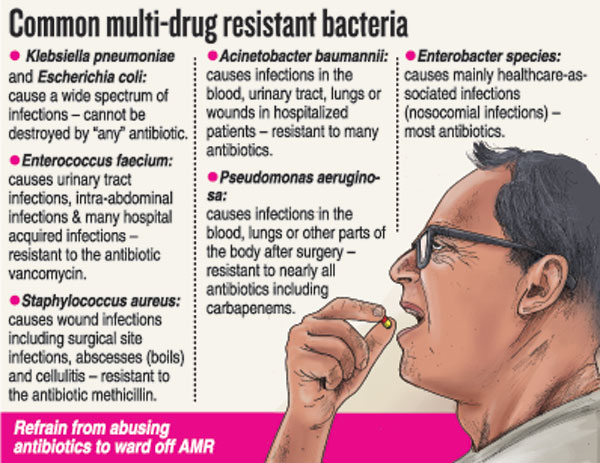
Looking at the development of new anti-microbial agents, she says that it is not very encouraging. Hardly any promising agents are in the pipeline even for the treatment of some common multi-drug resistant bacteria. Multi-drug resistant organisms (MDROs) are defined as micro-organisms, predominantly bacteria, that are resistant to one or more classes of anti-microbial agents.
She explains that even though certain names of MDROs describe resistance to only one agent (such as MRSA – Methicillin-resistant Staphylococcus aureus or VRE – Vancomycin-resistant Enterococci), these pathogens are frequently resistant to most available anti-microbial agents.
“The reasons for not producing new anti-microbial drugs include it not being profitable for drug companies, as these antibiotics become expendable after some time as bacteria become resistant to the newer antibiotics too. Another is that almost all options on producing antibiotics have already been used,” says this Microbiologist.
How can we stop the appearance of drug-resistant bacteria?
“The ‘only way’ out of this health dilemma is to reduce ‘irrational’ (wrong) use of antibiotics. Even then, we cannot ‘stop’, only slow down the appearance of resistant bacteria, said Dr. Abeywardena.
She shows the way on rational use of antibiotics:
- Take antibiotics only if they are prescribed by a qualified doctor who has diagnosed your illness correctly.
- Stop self-treatment with antibiotics by getting antibiotics over the counter for the common cold, sore throat, diarrhoea and chronic wounds. Coughs, colds, sore throats and diarrhoea are mostly caused by viruses which are self-limiting. Do not consider antibiotics to be quick-fix medications for all illnesses.
- Do not stop taking antibiotics when feeling better, but continue the full course. Many people suffer from recurrent urinary tract infections due to resistant bacteria because they have not completed the course of antibiotics during previous infection episodes.
- When on an antibiotic course, it is important to take the correct dose, at the correct time and for the correct duration.
- Do not reduce the dose of antibiotics hoping to reduce side-effects.
- Do not share antibiotics with family members with similar symptoms.
Referring to what drives AMR, Dr. Abeywardena says that practices in both healthcare settings and the community facilitate the emergence and spread of drug-resistant bacteria. In hospitals, there could be inappropriate prescription of antibiotics, improper usage of antimicrobials including wrong dosage and timing of administration and lack of antibiotic stewardship programmes.
| Situation in Sri Lanka About 25% of Escherichia coli and 70-100% of Acinetobacter species have been found to be resistant to most antibiotics, says Dr. Madhumanee Abeywardena, pointing out that Sri Lanka does not have much data on this critical issue. Explaining that the data available, though, indicate that 42%-86.5% of Staphylococcus aureus bacteria are resistant to commonly used antibiotics, she cautions that these antibiotic-resistant species are not limited to hospitals but also go among people and cause disease. Dr. Abeywardena quotes several Sri Lankan studies – A study at the National Hospital of Sri Lanka (NHSL) from June to August 2014 had found that:
A study at the Anuradhapura Teaching Hospital from August 1 to October 31, 2009 had found:
| |
| Go blue ‘Go blue for the AMR campaign’ particularly next Thursday (November 24), the World Health Organization (WHO) has urged. The Sri Lanka College of Microbiologists has invited its members to wear light blue and workplaces and facilities such as hospitals, clinics, laboratories, pharmacies and universities to light up their offices in blue. “Raise public awareness on the dangers of AMR brought on by the abuse and misuse of antibiotics,” adds the college |
The best way to say that you found the home of your dreams is by finding it on Hitad.lk. We have listings for apartments for sale or rent in Sri Lanka, no matter what locale you're looking for! Whether you live in Colombo, Galle, Kandy, Matara, Jaffna and more - we've got them all!

