News
What ails NHSL where patient-friendliness is compromised
View(s):
Staff behaviour towards patients remains problematic at the country's leading state hospital. Pix by Akila Jayawardena and Eshan Fernando
By Tharushi Weerasinghe
“I brought my wife on a wheelchair, and she kept expressing her discomfort and nausea, but hospital staff ignored my requests until my wife threw up—and even then they just brought a stretcher and told me to put her on it myself,” said a 50-year-old man. The vomit was not cleaned off the floor for the next two hours. He told the Sunday Times that this was in the presence of many nurses who were more interested in watching something at one of the reception desks than getting the floor cleaned.
Another patient had this to say: “The doctor gave me some medicines to take while at the OPD itself, but the dressing room did not have clean, filtered water. The nurse told me to drink straight from the tap in the sink. Neither the doctor nor the nurses told me about the medicines I was given.”
The 28-year-old patient from Thalawathugoda had come to get treatment for a hand injury. He observed that the door of the X-ray room was often kept open, though the accepted practice was to keep it closed to prevent the spread of radiation. The X-ray room is also being used as a storage room for old Vesak decorations.
When asked about these complaints, NHSL Director Dr. Indika Jagoda said, “The hospital does have a responsiveness issue, and that’s why we have installed surveillance cameras everywhere now.” He pointed to two CCTV screens on his desk showing various parts of the hospital.

NHSL Director Dr. Indika Jagoda
Dr. Jagoda said it was a struggle to even address minor deficiencies like buying paper cups, water dispensers, and clothes for accident ward patients. “We recently upgraded our tin-sheet trolleys to ones with mattresses, but we don’t have the allocation to buy sheets for the mattresses.”
Recently, the hospital received a donation of 1500 hospital gowns for patients to wear upon being admitted in bloodied or soiled clothes. He held that this was not due to a lack of funds but a difficulty in getting funds for innovation. “We have to justify it from scratch, which is difficult, so we opt for donors instead.”
The hospital has obtained new machines and furnished waiting rooms through state and private funds. However, patient care and staff attitudes still need improvement. While efforts like beautifying the triage area have been made, staff behaviour towards patients remains problematic.

NHSL Deputy Director Dr. Rukshan Bellana
Dr. Jagoda claims that the attitude problem is a result of staff being too tired. Many NHSL junior staff, often from distant districts, receive one day off every three days. Some work overtime to accumulate days off for travel, despite the recommended six-hour shifts, which can be exhausting.
Other hospital officials, however, claim there is a bigger disciplinary issue at play. “The apathy of workers towards patients is both a supervisory issue and a financial issue,” said NHSL Deputy Director Dr. Rukshan Bellana.
He alleged that the workforce got into “bad habits” during the COVID-19 pandemic and also during the economic crisis when food, transport, and gas supplies collapsed. “People got used to not working on time because rotations were introduced, and we were more lenient about punctuality.”

Health Ministry Secretary Dr. P.G. Mahipala
The deputy director held that management was struggling to convert staff performance back to pre-COVID standards as many junior workers have deviated from standard protocols and disciplines. He added that these workers were emboldened by trade union action.
Dr. Bellana blamed the authorities for giving too much leeway for healthcare workers to come and go as they please—a privilege that he believed workers were now exploiting to engage in multiple other jobs on the side while working at the hospital.
He said some attendants took bribes from patients for what they called “extra help,” like getting a bed in a ward.
Dr. Bellana said the hospital management’s hands were also tied, as much of the authority to take disciplinary action lay with the ministry. “No punitive action is taken by the ministry against workers who hide behind trade unions and refuse to do their jobs.”
Trade unions insist that worker discipline is tied to quality of life. “We acknowledge a general culture of indiscipline in the healthcare sector, and it should be corrected,” said the Chief Secretary of the Joint Health Workers Union (JHWU), Ven. Tempitiye Sugathananda Thero. However, he emphasised that addressing discipline without improving morale is unsustainable.
The JHWU highlighted that NHSL minor staff are overworked due to understaffing. NHSL has 10,000 staff, with 3,000 being minor staff. While one official acknowledged understaffing, another argued it was an issue of poor organisation. The JHWU leader said staff retired annually, but new recruitment was often limited to election campaigns every five years. “Health workers often work overtime due to understaffing and to supplement their low base salaries,” he said.
Most minor staff recruitment was often politically inclined. “Workers from whichever district the minister is from are given jobs for electoral interests, and that is why most of the minor staff are from Polonnaruwa, Badulla, Ampara, and Kalutara.”
While doctors and nurses have quarters, minor staff do not, and paying for lodging while also earning enough money to send home was virtually impossible on the salary given. On average, a minor staff worker earns around Rs. 24,000 a month and often does two or three jobs to sustain himself and his family.
Some travel from distant places. A worker who comes from Kalutara leaves as early as 2:45 a.m. for the 6:30 a.m. shift.
The JHWU leader said he had suggested district quotas for recruitment to allow more health workers to work in their home districts, a recommendation often ignored by authorities.
Unions also noted a lack of mental support for health workers, especially post-COVID. “These people were on the frontlines of a biological war and need rehabilitation from the strain they experienced.” Other issues impacting worker attitudes include the absence of a canteen and daycare facilities for minor staff within the hospital.
“We have no issue with welfare societies providing these services, as they do in other hospitals, but opening a daycare facility for less than 10 children makes no sense,” Health Services Director General Dr. Asela Gunawardene said.
He said state funding for such facilities was difficult as the priority remained patient care, especially at a time when funding for construction and repairs had been stalled for the last four years. “We only received funding this year, so we have to prioritise. If allocations are made in the next budget, we can undertake it.”
Dr. Gunawardene acknowledged that opening a canteen for every staff subsection is impossible, but a welfare canteen is a consideration. While old hospitals lack pantry rooms, this is a priority in new hospitals being built.
He also noted that it is administratively challenging for the department to consider factors like workers’ quarters when making government appointments. “Appointments for junior staff happen at the discretion of the minister, so it is out of my hands,” he added.
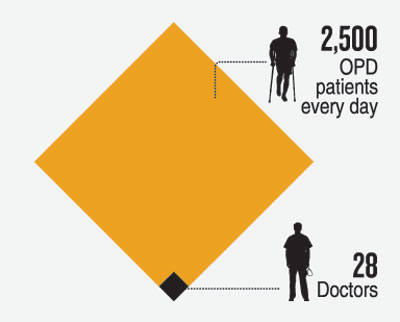
| Doctor migrations straining doctors who stay Doctor migration is an issue for the NHSL. “I need six months to train a new doctor and two years for them to be considered experienced, but we are struggling because about six nurses leave every week,” noted NHSL Director Dr. Indika Jagoda. Additionally, 28 doctors handle the daily influx of 2,500 OPD patients, leading to overburdening. In response, Health Ministry Secretary Dr. P.G. Mahipala said that 1,300 doctors are receiving peripheral appointments, and 450 more are completing training. In January, 2,200 nurses entered the system, and 1,000 midwives were absorbed for training. Dr. Mahipala added that health sector reforms aim to increase long-term job satisfaction. “Measures like the increase in Disturbance, Availability, and Transport (DAT) allowance were also taken to facilitate reforms and maintain staff numbers,” he said. ICU cleaned by janitorial staff, in violation of WHO protocol At the NHSL, the Intensive Care Unit (ICU) is cleaned by janitorial staff, instead of health workers, violating World Health Organisation infection prevention protocols. “This is happening because the professionals supposed to do it are refusing,” said NHSL Deputy Director, Dr. Rukshan Bellana. He added that NHSL is the only hospital in the country where this occurs. The risk of cross-contamination increases as janitorial workers clean the ICU in the same attire after cleaning other hospital areas, including toilets. Photos obtained by the Sunday Times show janitorial staff in the ICU without face masks. Dr. Bellana highlighted the high rates of post-transplant infections, particularly among liver and kidney transplant patients, at NHSL. He noted, “No official study has been done, but ICU hygiene cannot be ignored.” Dr. Bellana reported this issue to the Ministry 14 months ago, but it remains unresolved. “We have conducted preliminary inquiries; the authorities should either transfer or interdict these workers,” he urged. Health Services Director General Dr. Asela Gunawardene acknowledged that the issue is limited to NHSL. He said that ICUs and neonatal units in other hospitals are maintained by hospital staff.  Janitorial staff, instead of health workers clean the ICU “When a system has been in place for a long time, trying to correct it faces a lot of resistance,” he said, adding that the Health Ministry Secretary had appointed a committee to report on the matter for further action. The Sunday Times found that the committee led by Additional Secretary Dr. Lakshmi Somathunga submitted its findings over eight months ago., but little or no action has been taken to reinstate this vital health protocol. Dr. Somathunga was unavailable for comment. The regulation is clear: the ICU must be sterilised by certified health professionals under national and international | |
The best way to say that you found the home of your dreams is by finding it on Hitad.lk. We have listings for apartments for sale or rent in Sri Lanka, no matter what locale you're looking for! Whether you live in Colombo, Galle, Kandy, Matara, Jaffna and more - we've got them all!

