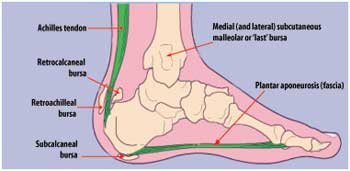
Plantar fasciitis means inflammation of the plantar fascia. The plantar fascia is a strong band of tissue (similar to a ligament) that stretches from the heel to the middle bones of the foot. It supports the arch of the foot. Small injuries to the plantar fascia can cause inflammation and symptoms. The injury is usually close to where it attaches to the heel bone.
What are the symptoms?
Pain is the main symptom. This can be anywhere on the underside of the heel. Commonly one spot is found as the main source of pain. This is often about four cm forward from the heel, and may be tender to touch. The pain usually eases on resting the foot, but is often bad when first used in the morning. Gentle exercise may then ease things a little as the day goes by, but a long walk or sudden stretching of the sole of the foot for example, walking up the stairs or on tip-toes may make the pain worse.
Who gets it?
Plantar fasciitis is quite common, mainly affecting the over-40s. It is more common in women and athletes. Situations where it is more likely to occur include the following.
- If you do lots of walking, running, standing, etc, when you are not used to it.
- Wearing shoes with poor cushioning.
- Sudden gains in weight or being overweight will put extra strain on the heel.
- Overuse or sudden stretching of the sole. For example: athletes who increase their running intensity or distance; poor technique starting 'off the blocks'; etc.
- Tightness of the Achilles tendon (at the bottom of the calf muscles above the heel).
 |
| Exercises for Plantar fasciitis |
Often there is no apparent cause, particularly in older people. A common myth is that the pain is due to a bony growth or 'spur' coming from the heel bone (calcaneum). Many people have a bony spur of the heel bone but this is not usually the cause of the pain.
What is the treatment ?
Usually the inflammation and pain will ease in time. Fascia tissue, like ligament tissue, heals quite slowly. However, the following measures may reduce the recovery to within weeks rather than months.
- Rest the foot as much as possible. Avoid running, excess walking or standing, and undue stretching of the sole. Gentle walking and exercises described below are fine.
- Footwear. Do not walk barefoot on hard surfaces. Choose shoes with cushioned heels and a good arch support. A laced sports shoe rather than open sandals is probably best. Avoid old or worn shoes that may not cushion the heel properly.
- Heel pads. You can buy various pads and shoe inserts to cushion the heel. These work best if you put them in your shoes at all times. Use soft materials. The aim is to raise the heel by about one cm. If the heel is very tender, cut a small hole in the heel pad at the site of the most tender spot. The tender part of the heel will not then touch anything inside the shoe at all.
- Painkillers such as paracetamol will help. Sometimes anti-inflammatory medicines such as ibuprofen which are not only painkillers but also reduce inflammation, may work better. Some people find that rubbing a cream or gel onto the heel that contains an anti-inflammatory medicine is helpful.
- Exercises. Regular gentle stretching of the Achilles tendon and the plantar fascia will help ease the symptoms. This is because most people with plantar fasciitis have a slight tightness of the Achilles tendon. This tends to pull at the back of the heel and have a knock-on effect of keeping the plantar fascia tight. Also, when you are asleep overnight, the plantar fascia tends to tighten up (which is why it is usually most painful first thing in the morning).
The following exercises will usually help.
- Stand 2-3 feet away from a wall. Keeping the knees straight and feet and heels on the ground, lean onto the wall. You should feel the calf muscles and the Achilles tendon tighten. Hold this position for several seconds then relax. Do this about 10 times. Repeat five or six times a day.
- Sit in a chair with the knees bent at right angles and the feet and heels flat on the floor. Now lift the foot upwards with the heel kept on the floor. Again you should feel the calf muscles and Achilles tendon tighten. This exercise uses a slightly different set of muscles to the above. Again, keep the position for several seconds then relax. Do this for about 10 times, five or six times a day.
The aim of the exercises is to gently loosen up the tendons and fascia above and below the heel. In one study, stretching exercises were rated as the most effective treatment.
- Injections. A steroid (cortisone) injection is sometimes tried if the pain is still bad despite the above measures. It may relieve the pain for several weeks, or even cure the problem. It is not always successful and may be sore to have done. Steroids work by reducing inflammation. Sometimes two or three injections are tried over a period of weeks if the first is not successful.
- Other treatments. Some people benefit from wearing a special splint overnight to keep the Achilles tendon and plantar fascia slightly stretched. The aim is to prevent the plantar fascia from tightening up overnight. (The splint does a similar job as the exercises described above.) In very difficult cases, sometimes a plaster cast is put on the lower leg. This provides rest, protection, cushioning and slight stretching of the plantar fascia and Achilles tendon. Athletes may find ice massage of the heel before and after exercise helpful.
- Surgery may be considered in very difficult cases. This is usually only advised if the pain has not eased after 12 months despite the treatments listed above. Surgery is not always successful. Surgery causes complications in some people so it should be considered a last resort.
(The writer is Consultant Rheumatologist, Sri Jayewardenepura General Hospital) |