Tuberculosis - for long counted among the most lethal infectious diseases in the world - has just become more dangerous. New strains of this virulent disease are becoming increasingly impervious to treatment with cases of Multi-Drug Resistant TB (MDR TB) being widely documented. Early this year, the World Health Organisation (WHO) upped the ante with a report detailing the global health risk posed by a lethal new form of drug resistant tuberculosis - Extreme Drug Resistant TB or XDR TB.
Also known as Extensive Drug Resistant TB, the outbreak has health authorities in over 49 countries (including neighbouring India) scrambling to nip it in the bud. The most efficient way to do so maybe to ensure that TB itself is treated properly.
Currently, tuberculosis claims three million lives a year globally, says Dr. Wijitha Senaratne, Consultant Chest Physician. However, those of us living in Sri Lanka can easily be forgiven for considering the threat posed by TB a little low on our list of priorities. After all, the island's successful TB control programme has ensured that we have one of the lowest prevalence rates in the region. In addition, Sri Lanka has also achieved the global targets for case detection and treatment success rate.
"But this is no reason to get complacent," warns Dr. Senaratne. At the Welisara Chest Hospital, Dr. Senaratne and his colleagues have come across patients who do not respond as expected to standard treatment. Their continued weight loss hints at what their phlegm tests reveal - that TB organisms are still flourishing inside them despite treatment.
Drug resistance:
a man made
phenomenon
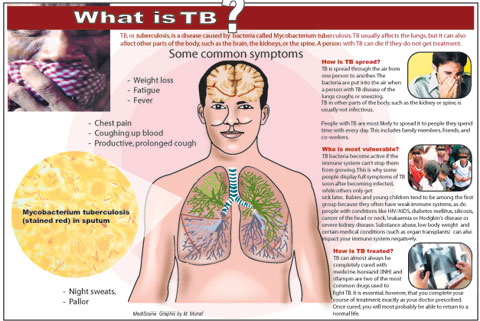
You can become infected by MDR TB just as you would with TB - by inhaling the MDR TB germs. These germs are put into the air when a person with TB coughs, sneezes, speaks, or sings. They can then float in the air for several hours, depending on the environment. Persons who breathe in the air containing these TB germs can then become infected. In addition, the organisms that create MDR TB are quite as infectious as regular TB, warns Dr. Senaratne.
However, those who are most at risk are known as defaulters. A percentage of patients with ordinary TB habitually stop their medication before the entire drug regimen is complete. These patients are known as defaulters and pose a grave risk to both themselves and others around them. Such defaulting is often attributed to the false sense of wellbeing patients experience a mere month or two into treatment. But, although they may no longer be displaying any symptoms, the organisms remain in their bodies.
In addition, patients with addictions to alcohol or drugs are also more likely to default on their treatment. The personal constraints experienced by those who live alone, or who are unable to travel to the clinic, also sometimes contribute to a patient defaulting.
Who else is vulnerable? "People who are at a risk of getting drug resistant TB, are patients who had TB in the past, and have now relapsed," says Dr. Senaratne. You can also contract it from exposure to someone who already has a drug resistant strain of TB. But in many cases, the very existence of drug resistant tuberculosis reveals a weakness in the management of their tuberculosis. "Drug resistance is always a man-made phenomenon," explains Dr. Senaratne, saying that in this case it is the result of misuse or mismanagement of anti-TB drugs. Sometimes patients do not either take their treatment regularly or complete the full course of treatment.
On the other hand, health-care providers may prescribe inadequate or sub optimal treatment regimens. Sometimes the supply of drugs is not constant or the drugs themselves are of poor quality.
When the drugs don't work
"The most important thing in the prevention of multi drug resistant TB, is to achieve a cure in ordinary TB - which means the patient must take the correct combination of drugs in correct doses, regularly, over the correct period." Early diagnosis and effective treatment kill two birds with one stone - the patient is saved, and a potential source of infection for the community is eliminated. "In TB, it is the cure that leads to prevention," emphasises Dr. Senaratne. In contrast, an inadequate or poorly implemented drug regimen will foster drug-resistant strains, which then proliferate, giving rise in turn to tougher strains. This cycle can perpetuate itself endlessly until the like of MDR TB is manifested.
He explains that MDR TB is TB that is resistant to at least two of the most effective anti-TB drugs, isoniazid and rifampicin. These drugs are considered "first-line drugs" - the first to be deployed because of their effectiveness. Unfortunately, in the treatment of MDR TB, doctors are forced to rely on second-line drugs which are not only less effective, but are more costly and more toxic than first-line drugs. Second-line treatment also requires that a patient be under medication for a longer period, says Dr. Senaratne explaining that the duration of treatment can be two years in contrast to the usual six months and is ideally accomplished under careful monitoring and supervision. Of course this is much easier said than done.
A global threat
"If a diabetic, asthmatic or hypertensive patient gives up and does not get his disease under control, it's his problem. In the case of TB, it's a community problem," says Dr. Senaratne. Now, it's becoming everyone's problem. In an increasingly globalised world, travel has made national boundaries porous - travellers now carry infectious diseases back to their own homes, while even a simple bus ride can expose you to the organisms that are transmitted by air. "Anyone who breathes air can get TB. Here, everybody's at risk," he says.
Like TB, MDR TB usually affects the lungs, but it can also affect other parts of the body, such as the brain, the kidneys, or the spine. 8,000 to 9,000 cases of TB are detected in Sri Lanka annually. In the past years, a small percentage of these have proved to be Multi-Drug Resistant. Unfortunately, some among these patients have defaulted on their medication or have had relapses. Such cases are more likely to develop XDRTB.
"Such patients are basically resistant to the second line drugs as well," says Dr. Senaratne, explaining that currently Sri Lanka does not have any recorded cases of XDR TB - possibly because we do not have access to expensive sensitivity tests required. We only know that those infected with XDR TB have MDR TB and are in addition resistant to second-line drugs - making them virtually impossible to treat. In the end, the development of MDR TB and XDR TB serve as timely reminders that the worst of the fight against tuberculosis may still lie ahead.
|