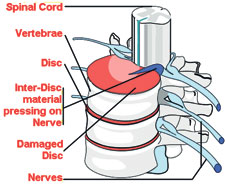
The spine is made up of many bones called vertebrae. These are roughly circular and between each vertebra is a 'disc', made of strong 'rubber-like' tissue which allows the spine to be fairly flexible. A disc has a stronger fibrous outer part, and a softer jelly-like middle part called the nucleus pulposus.
The spinal cord, which contains the nerves that come from the brain, is protected by the spine. Nerves from the spinal cord come out from between the vertebrae to take and receive messages to various parts of the body.
Strong ligaments attached to the vertebrae give extra support and strength to the spine. Various muscles also surround, and are attached to various parts of the spine.
What is a prolapsed disc?
When you have a prolapsed disc (commonly called a 'slipped disc'), a disc does not actually 'slip'. What happens is that part of the inner softer part of the disc (the nucleus pulposus) bulges out (herniates) through a weakness in the outer part of the disc. A prolapsed disc is sometimes called a herniated disc. The bulging disc may press on nearby structures such as a nerve coming from the spinal cord. Some inflammation also develops around the prolapsed part of the disc.
Any disc in the spine can prolapse. However, most occur in the lumbar part of the spine (lower back). The size of the prolapse can vary. Generally, the larger the prolapse, the more severe the symptoms.
Who gets a prolapsed disc?
Though, bouts of back pain are very common, less than 1 in 20 cases of acute (sudden onset) back pain are due to a prolapsed disc. Most are 'simple low back pain' thought to be caused by a minor problem to a muscle, ligament, or other structure in the back. The commonest age to develop a prolapsed disc is between 30 and 50 years. Twice as many men as women are affected.
What causes a prolapsed disc?
It is not clear why some people develop a prolapsed disc - they may have a weakness in the outer part of the affected disc. Various things may trigger the inner softer part of the disc to prolapse out through the weakened outer part of the disc. For example, sneezing, awkward bending, or heavy lifting in an awkward position may cause some extra pressure on the disc. In people with a weakness in a disc this may be sufficient to cause a prolapse.
Jobs involving lots of lifting, lots of sitting (especially driving), weight bearing sports (weight lifting, etc), smoking, obesity, and increasing age (a disc is more likely to develop a weakness with increasing age) may increase the risk.
What are the symptoms
of a prolapsed disc?
Back pain
The pain is often severe, and usually comes on suddenly. The pain is usually eased by lying down flat, and is often made worse if you move your back, cough, or sneeze.
Nerve root pain (usually 'sciatica')
Nerve root pain is one that occurs because a nerve coming from the spinal cord is pressed on ('trapped') by a prolapsed disc, or is irritated by the inflammation caused by the prolapsed disc. Although the problem is in the back, you feel pain along the course of the nerve in addition to back pain, down a leg to the calf or foot.
 |
| MRI scan showing disc prolapse |
Nerve root pain is often worse than the back pain. With a prolapsed disc, the sciatic nerve is the most commonly affected nerve. (The term 'sciatica' means nerve root pain of the sciatic nerve.) The sciatic nerve is a large nerve that is made up from several smaller nerves that come out from the spinal cord in the lower back. It travels deep inside the buttock and down the back of the leg. There is a sciatic nerve for each leg.
Other nerve root symptoms
Irritation or pressure on the nerve next to the spine may also cause pins and needles, numbness or weakness in part of a buttock, leg or foot. The exact site and type of symptoms depends on which nerve is affected.
Cauda equina syndrome -
rare, but an emergency
A particularly serious and rare type of nerve root problem, this can be caused by a prolapsed disc. Here the nerves at the very bottom of the spinal cord are pressed on, causing low back pain plus: problems with bowel and bladder function (usually unable to pass urine), numbness in the 'saddle' area (around the anus), and weakness in one or both legs. This syndrome needs urgent treatment to preserve the nerves to the bladder and bowel from becoming permanently damaged. See a doctor immediately if you develop these symptoms.
No symptoms?
Research studies where routine back scans have been done on a large number of people have shown that some people have a prolapsed disc without any symptoms. It is thought that symptoms mainly occur if the prolapse causes pressure or irritation of a nerve. This does not happen in all cases. Some prolapses may be small, or occur away from the nerves and cause minor, or no symptoms.
How does a prolapsed disc progress?
In most cases, the symptoms tend to improve over a few weeks. The bulging prolapsed portion of the disc tends to get smaller (regress) over time in most cases. The symptoms ease in many cases. In only about 1 in 10 cases is the pain still bad enough after six weeks to consider surgery.
Do I need any tests?
Your doctor will normally be able to diagnose a prolapsed disc from the symptoms and by examining you. (It is the common cause of sudden back pain with nerve root symptoms.) In most cases, no tests are needed as the symptoms often settle within a few weeks.
Tests such as x-rays or scans may be advised if symptoms persist. In particular, a MRI scan can show the site and size of a prolapsed disc. This information is needed if treatment with surgery is being considered.
Treatments
Exercise and keep going
Continue with normal activities as far as possible. As a rule, don't do anything that causes a lot of pain but be prepared to accept some discomfort. In the past, advice had been to rest until the pain eases. It is now known that this was wrong. You are likely to recover more quickly and are less likely to develop chronic (persistent) back pain if you keep active. Also, sleep in the most naturally comfortable position on whatever is the most comfortable surface.
Medication
If you need painkillers, it is best to take them regularly. This is better than taking them 'now and then' only when the pain is very bad.
Physical treatments
Some people visit a physiotherapist for manipulation and/or other physical treatments that may provide some short-term comfort and hasten recovery in some cases.
Surgery
Surgery may be an option for some cases and may be considered if the symptoms have not settled after about six weeks or so. This is only in a minority of cases.
The aim of surgery is to cut out the prolapsed part of the disc that eases symptoms. However, it does not work in every case. Also, as with all operations, there is a risk from surgery.
Can further bouts be prevented?
The best way to prevent bouts of back pain and prolapsed disc is simply to keep active, and exercise regularly by walking, running, swimming etc.
(The writer is a Consultant Rheumatologist) |