Unseen to the human eye, danger lurks everywhere, waiting to explode. It’s just a matter of time before the “pandemic” alarm is sounded again and the world braces for pestilence and disease which may very well leave millions dead.
In the past 10 years alone humans have been hit by diseases such as Severe Acute Respiratory Syndrome (SARS), avian or bird flu (H5N1) and most recently swine flu (H1N1) which kept the world on alert for a pandemic.
But behind closed doors, in high-tech laboratories, bent over microscopes and poring over gene sequences, scientists are in a race against time. Among them is none other than a soft-spoken and unassuming Sri Lankan who hit the headlines from his base in Hong Kong in 2003.
He is Prof. Malik Peiris, the SARS buster who came into the limelight when he and his team isolated the corona virus that was causing much concern as it spread rapidly across the globe.
In Sri Lanka for a holiday with his mother and other relatives in Kandy and also to speak to students under the first Meeting of Minds (MoM) series held in Colombo by the Hong Kong University, he is still the humble and simple researcher he was when the Sunday Times met him soon after his success in October 2003.
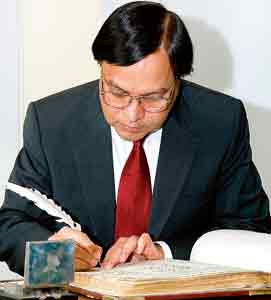 |
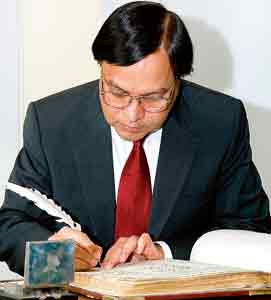
| Rare privilege: Signing the book after being elected a Fellow of the Royal Society of London.
Pic courtesy Royal Society |
The accolades and laurels seem to lie lightly on his shoulders and the accolades have been many…………..the first Sri Lankan to be elected a Fellow of the Royal Society of London in 2006, the highest scientific honour in the Commonwealth, the Chevalier de la Legion d’Honneur, France (2007) founded by Napoleon; the Mahathir Science Award, Akademi Sains, Malaysia (2007); and the Silver Bauhinia Star in Hong Kong SAR (2008). He and fellow scientist Prof. Guan Yi have also been featured in numerous publications including TIME Magazine’s ’60 Years of Asian Heroes’ in 2006. With 320 research publications and over 11,000 citations, 61-year-old Prof. Peiris is ranked as one of the top 1% most-cited international scientists worldwide by Essential Science Indicator of ISI. He is also President of the Asia Pacific Society of Medical Virology.
“I was scared that I might blot the page,” smiles Prof. Peiris who had to sign the book after being elected a Fellow of the Royal Society of London, the “most important moment” of the ceremony, for the nearly 400-year-old book had been signed by greats such as Isaac Newton (physicist, mathematician and astronomer who came up with the theory of gravity) and Charles Darwin (naturalist who dealt at length ‘On the Origin of Species’). The very first member of the Royal Society of London was physicist, chemist, inventor and natural philosopher Robert Boyle noted for the law after his name and only a select number are awarded this huge honour, after being nominated for outstanding contributions in science and research.
“I didn’t mess up the page,” says Prof. Peiris whose worry stemmed from the fact that a quill pen had to be used, while the Sunday Times understands that many nominees have to be on the “waiting list” for many long years before being bestowed the honour or rejected but this Sri Lankan scientist got it in just one or two years. The Royal Society of London, possibly the oldest “learned society” for science had been founded in November 1660 during the reign of King Charles II it is understood.
Viruses and how and why they jump from animals to humans causing new and emerging illnesses have been and are Prof. Peiris’s speciality.
There are many thousands of viruses, he says, explaining that he and his team are trying to understand the threats out there, to predict which might be important among domestic and wild animals that could become problematic for humans by jumping across species.
Talking about “exciting findings”, he flips back the pages of time to bring the influenza viruses into perspective. In 1968, 43 years ago, nobody knew from where these pandemic viruses came from or whether they were new viruses. In the 1970s Robert Webster identified that they were animal viruses and since then we have worked back, he says, pointing out that for 12 years his team of scientists and researchers have been studying the influenza virus in pigs. Having a head-start, with few others having such long-term systematic data on viruses in pigs, they published their findings on how the influenza virus changes in pigs, in the prestigious British magazine, ‘Nature’, when the swine flu (A/H1N1) pandemic hit in 2009.
Delving into scientific detail, Prof. Peiris says that 30-40 years of study worldwide had shown that the avian influenza virus jumped to pigs in Europe while in North America there had been a mixing of the swine, human and avian influenza viruses in 1998. “A hybrid of the North American and European viruses caused the pandemic swine flu.”
A “big area of research” he as Scientific Director of the HKU-Pasteur Research Centre and his team is currently engaged in is to understand what allowed this pandemic virus from pigs the capacity to transmit (pass on) in humans. They are using animal models, especially the ferret, to pinpoint which gene of the virus is contributing to transmissibility in humans.
The work had started much earlier when they were not only studying the SARS-causing virus to see what and how it had adapted to transmit firstly from animal to human and then from human to human but also looking at the big animal markets in China where all sorts of exotic animals are kept together, making viruses mix easily.
“These markets have more types of animals than the Dehiwela Zoo,” Prof. Peiris later tells awe-struck students during the MoM lecture.
The research gathered momentum when reports came that there was an “unusual outbreak of pneumonia” not affecting just one or two, but clusters of people, leaving one in 10 dead. The patients didn’t respond to the usual treatment with antibiotics. “It was frightening,” says Prof. Peiris.
By March 12, there was a global alert by the World Health Organization (WHO) and there was a race to identify the cause. Some researchers claimed it was the metapneumo virus while others said it was caused by the chlamydia bacteria. “We kept testing the throat swabs of those with this disease in Hong Kong using many different methods,” says Prof. Peiris.
Excitement mounted in the lab, as they spotted a virus isolated from the specimens of one SARS patient. But was it new? Events happened quickly thereafter. Blood from patients with SARS reacted with this newly-isolated virus indicating that they were on the right track. Going further, they fished for genes of this new virus and after 39 false starts, hit the jackpot. They then amplified a short fragment of nucleic acid of the offending virus, and when matching it with those present in global genetic sequence databases, found that it was related to the family of the corona virus – but it was a new one, not known previously.
Prof. Peiris remembers the night of March 21 clearly. “It was about 11 when we informed the WHO that we think we have isolated the cause of SARS,” he says with humility………. “hot off the press”.
How did humans get the corona virus? Studying civets brought enlightenment, for in those trapped in the wild and brought to these markets there was no evidence of the corona virus but those tested in the live animal markets had a SARS-like virus. This was a clear pointer that the virus had jumped from another species and civets were only acting as amplifiers to spread it.
What was the team’s next move? Stressing that education should not be just to get a job and future security, he points out that it should arm a person with problem-solving abilities. Thereafter, he advises, young researchers should be curious why something is happening one way or not another way.
When they realized that civets were only amplifiers, his team’s inquiring minds looked around at all the other animals. Curiosity and hard work paid off -- it was discovery time! They found the corona virus in bats but not creating a disease like SARS, although later other researchers in Hong Kong and Australia had reported a SARS-like corona virus in bats.
The conclusion was simple. The “grandfather” of the SARS virus was present in bats. This was what was transmitted to civets which became the “adapting room” which made it pass onto humans, he says.
Next, Prof. Peiris deals with the swine flu, which he says though it was mild spread rapidly like wildfire. It started around March 2009 in Mexico and by October, just six months later, infected half the children of Hong Kong, half-a-world away. “The world is very fortunate that it was mild. If it was even a bit more severe, we would have been in big trouble,” he says. Even though the swine flu virus is relatively mild, when millions of people are infected with any flu virus, a few get severe complications and some even die as happened in this case.
For Prof. Peiris, one looming threat, however, is avian flu (H5N1) which is still endemic in poultry in Indonesia, Vietnam, Bangladesh, parts of India, Egypt and some parts of China, with the most recent patient being diagnosed in South Korea and another in Hong Kong.
The virus has not learnt the trick of how to spread from human to human, he says, only from birds to humans. If it does, with a mortality rate of 50%, there will be a calamity. Of the 508 who contracted the disease worldwide, 302 died. While doing more research to understand why this virus is so lethal, Prof. Peiris says, they hope and pray it will not become a pandemic.
When asked whether looking back he has any regrets, Prof. Peiris laughingly says, “Professionally no, but personally….”
When the Sunday Times met him in 2003, he had expressed concern about not spending enough time with his family. The regret is still there as his daughter is now in England having gone on a completely different line. “She did drama and acting and has in fact acted in two plays there,” he smiles, adding that his son is doing his first degree in America as he is not sure what his career should be.
However, in December they all spent time together, he says, explaining that his wife, Shamala, has been a source of great support and encouragement not only in his work but also in handling their children.
His time-consuming work at the expense of his family has not been in vain. At the centre of dramatic developments and findings in the study of viruses, for Prof. Peiris it is all about saving lives.
How it all started: Tracing his career
The seeds of curiosity and determination to ascertain why, began for Prof. Peiris way back as a virologist of the University of Peradeniya, after having studied at St. Anthony’s College, Kandy, secured his medical degree from Peradeniya itself and undergone his postgraduate studies at the University of Oxford.
He was setting up the virology lab at the university when mosquito-borne Japanese Encephalitis (brain fever) began felling farmers, 503 to be exact in the Anuradhapura area from October-December 1985. Suddenly “out of the blue” there was a JE epidemic.
Like policemen looking for clues at a murder scene, they began their own “investigation” in Anuradhapura. He was working with the late Prof. Prashantha Amerasinghe, an expert on mosquitoes, Dr. Tilak Abeysekara who was treating the patients with the disease, Dr. Nihal Abeysinghe, the Epidemiologist, and researchers at the Medical Research Institute. With him also was his very first M.Phil student, Parakrama Perera.
There were almost 500 cases with over 10% fatalities and many of those who survived were also left with paralysis, he recalls.
The JE virus had been present in the area for a long time, with a few people falling victim on and off. But suddenly why were there such a large number of cases in one part of Sri Lanka?
Wild birds had transmitted the virus through mosquitoes to other birds and once again through mosquitoes to pigs. In pigs, the virus had got amplified and mosquitoes had once again given it to humans. Mosquitoes had been there in hordes in rice paddies in this region for many years. So what had been the trigger? Why now? What had changed? Had the virus undergone a change and produced a new strain? Had the mosquito numbers changed? Had the mosquito type changed?
They looked at the virus – there was no mutation. Setting mosquito traps, they caught around 10,000 at a time and screened them for the virus, but the type of mosquito carrying the virus had also not changed nor had the mosquito numbers because there were hordes in the rice paddies. What of the pigs? Numerous blood samples from pigs and still there was no explanation.
The answer became obvious awhile later. To supplement the protein intake as well as their income, the local authorities had provided backyard pigs to the farmers. It was a good idea but that was what set the match resulting in an explosion.
Just a change in eco conditions had sad consequences, says Prof. Peiris. But the scientists were able to prevent a similar “disaster” in the Mahaweli resettlement areas by advising the authorities not to provide the “vessel” which came in the form of pigs in areas of intensive rice cultivations. Whenever ecological changes are made it is important to have a risk assessment, he points out.
Tackling pandemic threats
A complete change is what Prof. Peiris is recommending with regard to the current vaccine production in the face of pandemic threats.
Not confining his work to researching viruses, he has become proactive in attempting to create a volte face in this regard, for the vaccine for swine flu (H1N1) came too late for those in Hong Kong……..and it was over a drink and a chat on old times (JE in A’pura) three years ago in Washington that he discussed the matter with none other than his first M.Phil student Parakrama Perera now working at the National Health Institute (NIH) on developing a vaccine to fight cancer and tuberculosis.
If a pandemic hits, the production regimen of six months will be futile. The most urgent challenge is to protect against not one but all sub-types of influenza, H1 to H16, says Prof. Peiris holding out hope.
We are working out a strategy similar to what Parakrama is working on for influenza as well, he adds. “We can then manufacture it in bulk and stockpile it to save lives.” |