KINGS HOSPITAL INTRODUCES THE CONCEPT OF GERIATRIC MEDICINE, ESPECIALLY TAILORED FOR ELDERLY PATIENTS
"IN A NOVEL
move in Sri Lanka, Kings Hospital is setting a new standard in elderly care with the introduction of a specialized Geriatric Medicine concept. Dr. Kelum Pelpola, an expert in this field, has pioneered this initiative, bringing a wealth of knowledge and experience from his extensive training and practice in the UK. With a holistic approach tailored to the unique needs of older adults, Dr. Pelpola and his team aim to enhance the quality of life for elderly patients through comprehensive, individualized care. In this insightful Q&A, Dr. Pelpola delves into the nuances and benefits of Geriatric Medicine, explaining why this specialty is crucial for our ageing population."
Q: Could you tell us about your background and expertise in Geriatric Medicine?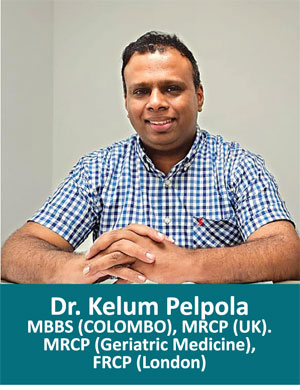
A: I graduated from the Faculty of Medicine in Colombo and pursued postgraduate studies in the UK, training in the East of England Deanery. I became a Consultant in General Medicine and Geriatric Medicine (dual accredited), and worked at the Norfolk and Norwich University Hospital, one of the UK’s largest hospitals. I later served as the Service Director/Head of Department for Geriatric Medicine at this hospital. This role involved overseeing care for a large number of elderly patients, and the hospital had around 20 Geriatricians working in different subspecialties of Geriatric Medicine.
I am also a member of the British Geriatric Society and a Fellow of the Royal College of Physicians in London.
In the UK, Geriatricians handle all patients over 65 with medical problems, whereas a similar model has been in place for a number of years in countries like the Australia, New Zealand, and the US too.
Q: Can you introduce what Geriatric Medicine is and why it is necessary?
A: Geriatric Medicine, much like Paediatrics is for children, is a specialized field focused on the healthcare of older adults. This specialty has been around for some time in European countries like the UK, as well as USA and Australia. It recognizes that older people often have multiple, complex health issues simultaneously. For instance, while younger people may only deal with a single health issue like an infection or a heart condition, older adults might have heart problems, lung issues, kidney concerns, and more all at once. This complexity requires a nuanced approach because treating one condition can adversely affect another. For example, treating the heart might worsen kidney function, and vice versa. Moreover, older adults are more susceptible to medication side effects. They also have issues like diabetes, high blood pressure, and cholesterol, which complicate treatment for other conditions.
Q: Is there an age cut-off for when someone should start seeing a Geriatrician?
A: Generally, the age cut-off is around 60 to 65 years, though this can vary by region. In some areas, like certain hospitals in the UK, the cut-off might be higher, due to the sheer volume of elderly patients. Typically, though, most places consider 65 as the starting age for geriatric care.
Q: What are the most common health problems seen in the elderly population?
A: Common health issues in the elderly include osteoporosis, which leads to weakened bones and a higher risk of fractures, especially in the hip, wrist, and spine. Urinary and bowel incontinence are also prevalent, along with memory problems such as dementia and delirium. Dementia encompasses various types like Alzheimer’s, Vascular Dementia, and Mixed Dementia. Additionally, older adults often face joint problems, depression, anxiety, and sensory impairments, such as poor vision and hearing, which increase the risk of falls and injuries.
Q: What benefits does this Geriatric Medicine concept offer to patients?
A: The primary benefit is a holistic approach to healthcare. Instead of focusing on individual conditions, we look at the patient as a whole, considering how treatments for one issue might affect other health concerns. This comprehensive care plan improves the patient's overall quality of life. For instance, rather than prescribing numerous medications from various Specialists, a Geriatrician assesses which medicines are truly necessary, sometimes even reducing the total number of medications. This process, called “de-prescribing”, can significantly enhance a patient’s quality of life by minimizing undesired side effects and drug interactions.
Q: Can you elaborate on the importance of de-prescribing in Geriatric Medicine?
A: De-prescribing is crucial because many older adults take multiple medications from various Specialists. This polypharmacy can lead to adverse effects and interactions, mainly in the elderly. By carefully reviewing each medication, Geriatricians can attempt to reduce the number of drugs a patient takes. It needs to be remembered that this cannot be done for all patients at all times, but can be done for the majority. This concept must be tailored for each individual that we see. For example, I've seen patients on blood pressure medications for decades whose conditions have changed over time, allowing us to safely reduce or stop some medications. This tailored approach not only improves health outcomes but also enhances the patient’s day-to-day life.
Q: How does Geriatric Medicine integrate with other specialties for conditions like cancer?
A: In cases like cancer, Geriatricians work closely with Oncologists to develop a treatment plan that considers the patient’s overall health and other medical conditions. This collaborative approach ensures that treatments like chemotherapy or radiotherapy are appropriate and manageable, improving the patient’s comfort and quality of life. We also engage in advanced care planning, which involves discussing future health scenarios and making decisions in advance, considering the patient’s and family’s wishes alongside medical recommendations.
Q: What role do allied health professionals play in geriatric care?
A: Allied health professionals like physiotherapists and speech therapists are integral to geriatric care. Physiotherapists help prevent falls and improve mobility through specific exercises. Speech therapists assist post- stroke patients and patients with dementia who have swallowing and communication issues. By collaborating with these specialists, we can address a wide range of issues comprehensively and improve the patient’s overall well-being.
Q: How has the parent-child relationship affected the health of elderly people in Sri Lanka?
A: In Sri Lanka, recently many children have migrated abroad, in some instances leaving their elderly parents to live alone. This isolation can exacerbate issues like depression and anxiety. Even when children are present, they often have demanding day jobs, leaving little time to care for their parents. This situation highlights the need for specialized geriatric care to support the elderly in maintaining their health and quality of life.
Q: Do you have special facilities here to practice the geriatric concept?
A: Geriatric Medicine is a relatively new specialty in Sri Lanka, with only a few specialists currently practicing, in the state and private sector. However, we are working to establish comprehensive care that includes physiotherapists and other therapists to provide a holistic review of patients' needs. My approach involves not just addressing a single issue but considering the overall health and well-being of the patient.
Q: How do you see the growth potential of people accepting this concept of Geriatric Medicine in our country?
A: There is significant potential for growth in Geriatric Medicine in Sri Lanka. As people live longer, there is a growing need for specialized care to maintain their quality of life. The concept of holistic, comprehensive care for the elderly is gaining acceptance, and I believe it will continue to expand, providing better health outcomes for our ageing population.
As the population ages, the need for specialized geriatric care becomes increasingly evident. Dr. Kelum Pelpola's introduction of this innovative concept at Kings Hospital, marks a significant step forward in addressing the complex health issues faced by older adults. Through a holistic approach that integrates various specialties and focuses on the overall well-being of patients, Geriatric Medicine promises to improve both the quality and longevity of life for the elderly. The acceptance and growth of this specialty in Sri Lanka could lead to a transformative shift in how we care for our ageing population, ensuring that they receive the compassionate, comprehensive care they deserve. With experts like Dr. Pelpola leading the way, the future of Geriatric Medicine in Sri Lanka looks promising.
-
Still No Comments Posted.
















Leave Comments