When the womb needs to come outWhat is a hysterectomy? Dr. Melanie Amarasooriya explains in our continuing series on common surgical procedures A 50-year-old school teacher and mother of three, Sujatha had been having heavy periods for some years. Initially she ignored it, but when she started feeling lethargic and sleepy all the time, she consulted her family doctor. Her haemoglobin level was found to be low and as the cause for this was suspected to be the heavy menstrual bleeding, she was referred to the gynaecology clinic at the nearest government hospital. There, the gynaecologist took her history and did a general examination, followed by an abdominal examination and a vaginal examination. Her womb was found to be enlarged, possibly due to fibroids. She was referred for an ultrasound scan of the abdomen and pelvis, which confirmed the presence of several fibroids in the womb.
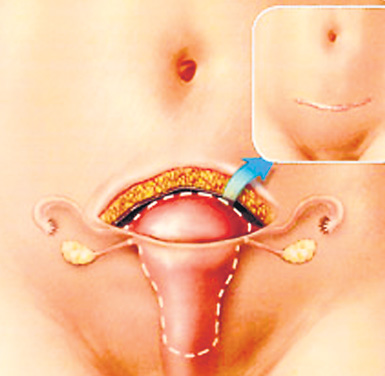
The medical team wanted to confirm that the cause of the anaemia was fibroids leading to heavy menstrual blood loss. A few other investigations were also carried out to rule out other causes. Sujatha was worried whether the fibroids in her womb meant cancer but the gynaecologist reassured her that fibroids are just harmless growths, that are common, even in young women. "Do I need to undergo surgery and get my womb removed?" Sujatha asked, having seen a friend undergo hysterectomy or surgical removal of the womb for fibroids recently. "It's not always necessary, but for you, I think it is the best option," he explained. Hysterectomy is one of the commonest gynaecological operations performed today, with the indications being heavy menstrual blood loss not responding to medication, fibroids, prolapse of the womb through the vagina or cancer, which is quite uncommon. For cancer, the definitive treatment is hysterectomy with or without other treatment modalities like chemotherapy or radiotherapy. However, for harmless growths like fibroids too the definitive treatment is removal. In a young patient, the uterus is conserved, removing only the fibroids. But this is a major surgery, with a higher rate of complications. Therefore, for a patient who is close to menopause, the safer option is total abdominal hysterectomy. For heavy periods where no organic cause can be diagnosed, medication can also be used, failing which the patient and the doctor can decide on surgical methods. For Sujatha, who had multiple large fibroids causing significant bleeding causing anaemia, the treatment of choice was surgery. And because of her symptoms treatment was fairly urgent. The gynaecologist explained that they would assess her suitability for major surgery, and also correct the haemoglobin level, while controlling the bleeding with medication for a while. As she was not anaemic to the extent of needing blood transfusions, she was prescribed iron tablets, medication to control bleeding and given a date for surgery. The doctor explained that once the womb was removed, she would have surgical menopause, which is menopause brought about by the surgery. She would not have menstrual periods. Since the ovaries would be removed, the hormones produced by the ovaries would also be deficient and she would have all the symptoms of menopause. She could also experience hot flushes and other problems like a normal menopausal woman. Sujatha wanted to know why her ovaries had to be removed."Even if we do not remove the ovaries, you will have the same problem, in another 1 or 2 years when you undergo natural menopause, when your ovaries cease to function. But if any problems arise from the ovaries, if we keep them, it is technically difficult to remove them after one surgery," the gynaecologist explained. "Also whenever you have a tummy problem hereafter, you will have to undergo scans and various tests to check whether it is a ovarian problem. In a younger woman, of say 40, we try to preserve ovaries for menopause is about 10 years ahead, but in someone closer to menopause, removal of ovaries at the same surgery is recommended." "You can take hormone replacement therapy (HRT) for symptoms of menopause, but it is not just an over the counter pill. It has its advantages as well as the side effects, so we need to assess you for suitability and only after weighing the risks and the benefits will you be a candidate for this treatment," he added. Sujatha was admitted for the surgery the day before the given date and assessed by an anaesthetist. Her haemoglobin level was checked before the surgery. Since she was 50, the doctors needed to assess her blood sugar level. An ECG was also taken to assess the heart. Blood was grouped, cross matched and saved in case of an emergency. The surgery was performed under general anaesthesia and an epidural catheter inserted through the backbone to control pain once the patient regained consciousness. The next morning she could walk to the bathroom and take a few steps within the ward. Patients are encouraged to resume their normal daily activities as soon as possible. Regaining mobility is particularly important since it helps to prevent complications, such as blood clots and pneumonia that could otherwise occur. However, she was constipated, quite a common problem after pelvic surgery. It improves with laxatives and increasing the amount of water, fruits and vegetables you take. Since there were no significant complications she could leave the ward on the 4th post operative day. On discharge, she was prescribed oral pain killers. A few patients do have complications, depending on the condition for which they undergo hysterectomy. Those are unexpected bleeding, accidental damage to other organs like urinary bladder or the ureter. Infections can also complicate this as in any surgery. Sujatha resumed normal work after two weeks. But this time may vary depending on each patient's condition. Patients should not exert themselves and should avoid lifting heavy weights (over 9 kg) for about six weeks. Sexual intercourse should also be avoided for the same duration to minimize the strain on healing tissues. Patients should seek medical advice if they experience pain that is not relieved with medication, persistent nausea or vomiting, bleeding heavier than a menstrual period, fever more than 101º F or 38º C, foul-smelling vaginal discharge, or inability to empty the bladder or bowels.
|
|
||||||
|| Front
Page | News | Editorial | Columns | Sports | Plus | Financial
Times | International | Mirror | TV
Times | Funday
Times | Medi Scene || |
| |
Reproduction of articles permitted when used without any alterations to contents and a link to the source page.
|
© Copyright
2008 | Wijeya
Newspapers Ltd.Colombo. Sri Lanka. All Rights Reserved. |